Switching a patient from a brand-name NTI drug to a generic version isn’t just a pharmacy transaction. It’s a clinical decision that can make or break treatment. NTI drugs - like warfarin, levothyroxine, phenytoin, and digoxin - sit in a dangerous sweet spot. Too little, and the condition returns. Too much, and the patient risks serious harm or even death. The difference between safety and disaster can be as small as a few nanograms per milliliter in the bloodstream.
Here’s the hard truth: even though the FDA approves generic NTI drugs as therapeutically equivalent, patients and even some providers still worry. A 2017 survey found that 40% of pharmacists hesitated to switch patients on NTI drugs, even though 94% believed generics were safe. Why? Because stories stick. A patient had a seizure after switching from brand to generic carbamazepine. A senior had an INR spike after switching warfarin brands. These aren’t myths - they’re real events that fuel fear.
Why NTI Drugs Are Different
Most medications have a wide safety margin. Take amoxicillin - you can take a little more or less and nothing dramatic happens. NTI drugs don’t play that way. Their therapeutic window is razor-thin. For example:
- Warfarin: Target INR is 2-3. An INR of 4.5 means bleeding risk. An INR of 1.5 means clotting risk.
- Digoxin: Therapeutic range is 0.5-0.9 ng/mL. At 1.2 ng/mL, you’re in toxic territory.
- Levothyroxine: A 12.5 mcg change can throw a stable thyroid patient into hyper- or hypothyroidism.
- Phenytoin: Levels below 10 mcg/mL may not control seizures. Above 20 mcg/mL, you risk dizziness, slurred speech, or worse.
The FDA requires stricter bioequivalence standards for these drugs. While regular generics must match brand drugs within 80-125% of absorption, NTI generics must stay within 90-111.11%. For levothyroxine, the bar is even higher - 95-105% for AUC. These aren’t arbitrary numbers. They’re based on real-world data showing what’s safe for patients.
What Patients Really Fear
When you tell a patient, “We’re switching you to a generic,” they don’t hear “same medicine.” They hear:
- “Is this cheaper because it’s weaker?”
- “Will I have another seizure?”
- “Did my doctor just cut corners?”
- “What if this kills me?”
These aren’t irrational fears. They’re rooted in real consequences. A 2018 Harvard study found that 8-12% of patients with well-controlled epilepsy had breakthrough seizures after switching to a generic antiepileptic. That’s not a lot - but for those patients, it’s everything.
Patients also don’t know that generics aren’t all the same. Two different generic versions of phenytoin can have different fillers, coatings, or release profiles. That’s why the FDA insists on tighter testing - but patients don’t know that. They just know they got a different-looking pill and now feel off.
How to Talk to Patients - The Right Way
Don’t say: “This generic is the same.”
Say this instead:
“I’m switching you to this generic version because it’s been tested to deliver the exact same amount of medicine into your bloodstream as the brand. We know this because the FDA required it to meet stricter standards than regular generics. I’ve prescribed this same generic to my own family members. But because this medicine works in such a narrow range, we’re going to check your blood levels in one week to make sure everything’s still on track. That’s just how we keep you safe.”
That’s not just information - it’s reassurance wrapped in expertise. You’re not just telling them it’s safe. You’re showing them you’re watching out for them.
Use the “librarian vs. advisor” rule. The librarian just reads the facts. The advisor connects those facts to the patient’s life. Say: “I know you’ve been stable for two years. We’re not changing your dose. We’re just changing the pill you take - and we’re going to double-check that it’s working just as well.”
What to Do After the Switch
Communication doesn’t end when the prescription is filled. Monitoring is non-negotiable.
- For warfarin: Check INR within 3-5 days after the switch. Some patients need a second check at day 7.
- For levothyroxine: Check TSH in 4-6 weeks. Don’t wait longer.
- For phenytoin or carbamazepine: Check serum levels within 7-10 days.
- For digoxin: Monitor for nausea, visual changes, or irregular heartbeat - and check levels if symptoms appear.
Don’t assume the patient will report symptoms. Many don’t. Elderly patients, especially, may think dizziness or fatigue is just “getting older.” Be proactive. Call them. Ask: “How are you feeling since we switched?” Don’t wait for them to come to you.

Know Your State Laws
In 27 states, you can’t just switch an NTI drug without permission. Fourteen states require written patient consent before substitution. In some, pharmacists must notify the prescriber. In others, the patient must sign a form acknowledging the switch.
Don’t guess. Check your state’s pharmacy board website. If you’re in New York, you need a signed consent. In Texas, you can switch but must document the counseling. In California, you can’t switch at all without the prescriber’s OK for certain NTI drugs.
Document everything. Write in the chart: “Patient counseled on therapeutic equivalence of generic [drug] to brand. Advised to monitor for [symptoms]. INR/TSH/serum level to be checked on [date]. Educational materials provided.”
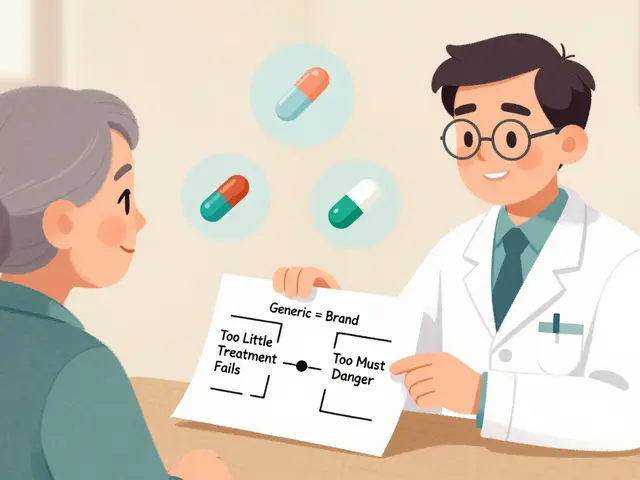
Use Visuals - They Work
Patients remember what they see. A 2023 survey found that pharmacists who used simple visual aids - like a scale showing the narrow therapeutic window, or a graph comparing brand and generic absorption - had 42% higher patient adherence.
Draw a line on paper. Label one end “Too little - treatment fails.” Label the other “Too much - danger.” Put a tiny dot in the middle: “This is where the medicine needs to be.” Then say: “The generic we’re using? It lands right here. Just like the brand.”
Or show a side-by-side image of the brand and generic pill - same shape, different color. Say: “Same medicine. Different color. Same result.”
What Not to Say
Avoid these phrases:
- “It’s just a generic.” (Implies inferiority.)
- “It’s cheaper.” (Makes them think quality dropped.)
- “The FDA says it’s fine.” (Too distant. They don’t trust bureaucrats - they trust you.)
- “Most people don’t notice a difference.” (What if they’re the one who does?)
Instead, say: “We’re doing this because it’s safe, and we’re going to make sure it’s working for you.”

When Not to Switch
There are times you shouldn’t switch - even if the generic is approved.
- Stable patient with no history of issues - leave them alone.
- Patient has had a bad reaction to a prior generic switch - don’t try again.
- Older adults on multiple meds - higher risk of interaction or absorption changes.
- Patient with renal or liver disease - their body may handle the generic differently.
- Patient is anxious or distrustful - wait until trust is built.
Don’t switch just because the insurance company wants it. If the patient is doing well on the brand, and the cost difference is small, keep them on it. Safety beats savings.
The Bigger Picture
NTI drug generics make up only 3.2% of all generic approvals - but they cause 11.7% of patient questions about generics. That’s because people are scared. And rightly so. The stakes are high.
But here’s the good news: when patients are properly counseled, problems drop by 28%. When pharmacists spend 10 full minutes explaining the switch - using teach-back methods to confirm understanding - adherence improves. Real-world data from the FDA’s 2024 pilot program shows that with clear communication, generic NTI drug use rises without increasing adverse events.
This isn’t about pushing generics. It’s about protecting patients. Every time you talk to a patient about switching an NTI drug, you’re not just filling a prescription. You’re preventing a crisis.
Be the person who doesn’t just hand over a pill. Be the person who checks in. Who asks how they’re feeling. Who draws the line on the paper. Who says, “I’m watching you.” That’s how you turn fear into trust.
Are generic NTI drugs really as safe as brand-name ones?
Yes - but only if they meet the FDA’s stricter bioequivalence standards. For NTI drugs, generics must deliver the same amount of medicine into the bloodstream as the brand, within a much tighter range (90-111.11%) than regular generics. The FDA tests these drugs more rigorously. Drugs like warfarin, levothyroxine, and phenytoin have specific guidelines that manufacturers must follow. When approved, they are therapeutically equivalent. But safety also depends on proper monitoring after the switch.
Why do some patients have problems after switching to a generic NTI drug?
Problems aren’t usually caused by the generic being ineffective - they’re caused by changes in absorption, timing, or patient perception. Even small differences in how the pill is absorbed - due to fillers, coatings, or manufacturing - can push a patient outside their therapeutic window. Also, patients may stop taking the medication if they think it’s “not working” because it looks different. That’s why monitoring and counseling are critical. A 2018 study found 8-12% of epilepsy patients had breakthrough seizures after switching, but many of those cases were linked to missed doses or lack of follow-up, not the drug itself.
Do I need to check blood levels every time I switch NTI generics?
Yes - always. Even if the patient has switched before without issues. Each generic version can behave slightly differently. For warfarin, check INR within 3-5 days. For levothyroxine, check TSH in 4-6 weeks. For phenytoin or carbamazepine, check serum levels within 7-10 days. Don’t wait for symptoms. Proactive monitoring prevents emergencies.
Can I switch a patient on multiple NTI drugs at once?
No. Never switch more than one NTI drug at a time. If a patient is on both warfarin and levothyroxine, switch one, monitor it for weeks, confirm stability, then consider the other. Changing two at once makes it impossible to tell which drug caused a change in symptoms or lab values. This is a common error that leads to avoidable complications.
What if my patient refuses to take the generic?
Respect their decision. If a patient is stable and concerned, don’t force the switch. Explain the benefits, show them the data, and give them time. Offer to recheck in a month. Some patients will agree after a conversation. Others won’t - and that’s okay. The goal isn’t to save money at all costs. It’s to keep them safe and compliant. If they trust the brand and are doing well, staying on it is the right choice.
Are there any NTI drugs that should never be switched?
There’s no official list of “never switch” NTI drugs. But in practice, avoid switching patients who are elderly, have kidney or liver disease, take multiple interacting medications, or have a history of instability after a prior switch. Also, if a patient has been stable for years on a brand-name drug with no issues, switching offers little benefit and adds risk. The FDA doesn’t forbid switching - but good clinical judgment says: if it ain’t broke, don’t fix it.
What Comes Next
The FDA is launching real-world monitoring in 2025 using data from 12 million patients to track outcomes after brand-to-generic switches. That’s a big step. But right now, the most powerful tool you have isn’t a database - it’s your voice.
Every time you sit down with a patient and explain why you’re switching their NTI drug - and then follow up - you’re not just doing your job. You’re preventing hospitalizations, seizures, strokes, and deaths.
Don’t let the fear of a rare problem stop you from doing the right thing. But don’t skip the steps that make it safe. Talk. Monitor. Document. Follow up. That’s how you turn a pharmacy decision into a patient safety win.

Ed Di Cristofaro
January 31, 2026 AT 16:29Man, I swear half the docs out here don’t even know what NTI means. I saw a pharmacist switch my grandma’s levothyroxine last month and she was dizzy for a week. She thought it was ‘just aging’-until she almost passed out in the grocery store. Don’t just say ‘it’s the same.’ Show them the data. Draw the line. Talk like they’re human.
Sami Sahil
February 1, 2026 AT 01:20Brooo this is lit!! 🙌 I work in a clinic in Delhi and we switch generics ALL the time. Patients freak out but once we show em the FDA graph? They chill. One old guy cried when he realized his pill wasn’t ‘fake’-just cheaper. Teach back = trust. Also, use the word ‘we’ not ‘you.’ Like ‘we’ll check your TSH in 4 weeks’-makes it feel like a team effort. ❤️
Deep Rank
February 2, 2026 AT 16:25Okay but let’s be real-how many times have you seen a patient actually *follow up* after a switch? Like, really? The system is broken. We tell them to check INR in 5 days, they get a text reminder, they ignore it, then they show up at the ER with a hemorrhage. And now we’re supposed to ‘draw lines on paper’ like we’re kindergarten teachers? This isn’t about communication-it’s about systemic neglect. The real problem isn’t the generic-it’s that nobody has time to care.
And don’t even get me started on how pharmacies get paid per switch. It’s a profit play disguised as cost-saving. We’re not saving lives-we’re hitting quotas.
Bryan Coleman
February 3, 2026 AT 01:48Good post. Real talk: I’ve been doing this for 15 years. I’ve seen zero deaths from FDA-approved NTI generics. But I’ve seen *dozens* of hospitalizations because people didn’t get monitored. The issue isn’t the drug-it’s the follow-up. I always say: ‘I don’t care what pill you take-I care that you’re alive next week.’ And I call them. No exceptions. Even if they’re 82 and say ‘I’m fine.’ I call anyway.
Also-yes, the fillers matter. One generic of phenytoin had a weird coating that slowed absorption. Took us 3 months to figure it out. So yeah, check levels. Always.
Naresh L
February 4, 2026 AT 13:58It’s interesting how we treat NTI drugs like they’re sacred, while ignoring the fact that every pill is a chemical negotiation between molecule and body. The ‘therapeutic window’ is a human construct-biology doesn’t care about our labels. Maybe the fear isn’t about generics-it’s about our illusion of control. We want to believe medicine is predictable. But it’s not. That’s why we need the check-ins-not because the drug is dangerous, but because we’re fallible.
Still, I agree with the advice. Draw the line. Talk slowly. Listen. Sometimes the pill is the easy part.
Ishmael brown
February 5, 2026 AT 14:31Okay but… what if the ‘brand’ is just a placebo? 🤔 Like… what if the patient’s ‘stability’ is just because they’ve been on it for 10 years and their brain thinks it works? I’ve had patients on brand-name warfarin for a decade who had no idea the generic was identical. Then we switched-same INR, same energy, same life. But they cried. Like they lost a pet. 😭
Maybe the real problem isn’t the drug… it’s the myth we’ve built around the brand logo.
June Richards
February 7, 2026 AT 13:36LMAO this is why medicine is a joke. You’re telling me we need to ‘draw a line on paper’ for patients to understand bioequivalence? And you’re surprised people don’t trust the system? If you had to explain this much just to give someone a pill, maybe the system shouldn’t allow switching at all. Just keep charging $500 for the brand. At least then you’re not risking lives for a $2 savings.
Lu Gao
February 9, 2026 AT 11:31Actually, the FDA’s 90–111.11% range is based on 2010–2014 data from 12,000 patients. The newer 2024 pilot showed *zero* increase in adverse events when counseling was done properly. So… your fear is statistically unsupported. But hey, I get it. People fear what they don’t understand. That’s why the ‘librarian vs. advisor’ thing works. You’re not just giving info-you’re building agency. 🙌
Chris & Kara Cutler
February 9, 2026 AT 23:07YES. Draw the line. 😍 I did this with my dad’s digoxin last year. He was terrified. I printed a picture of the pill, drew the line, and said, ‘This is where you need to be.’ He cried. Then he hugged me. We checked his levels. Perfect. He’s been fine for 8 months. You’re not just saving money-you’re saving trust. 💪❤️
Rachel Liew
February 10, 2026 AT 15:46i just wanted to say thank you. my mom is on warfarin and i was so scared to switch her. this post made me feel like i could do it right. i used your words exactly. i said ‘we’re going to check your INR next week’ and she said ‘okay, i trust you.’ that meant everything. you helped me be a better daughter.
Lisa Rodriguez
February 11, 2026 AT 13:44Just had a patient today ask if the generic was ‘the same as the one in the commercials’… I laughed and said ‘No, but it’s the same as the one in your blood.’ Then I showed her the graph. She got it. We did the check-up. She’s good. This stuff works. Don’t overcomplicate it. Just talk. Listen. Follow up. That’s all.
Nicki Aries
February 11, 2026 AT 15:38Let me just say… I’ve been a pharmacist for 22 years. I’ve seen patients switch from brand to generic, and then come back six months later, furious, because their ‘new pill’ made them ‘feel weird.’ But when we checked their levels? They were perfect. They’d stopped taking it because they didn’t like the color. So yes-counseling matters. But also… sometimes, the pill is just a symbol. And if the symbol gives them peace? Maybe… just maybe… you should let them keep it.