Topical Steroid Risk Calculator
Assess your risk of skin atrophy and infections
Using a strong steroid cream for a stubborn rash might seem like a quick fix-but what if it’s making your skin worse over time? Many people don’t realize that even short-term use of topical corticosteroids can lead to skin atrophy, thinning that doesn’t always show up right away but can become permanent. And when the skin barrier breaks down, infections follow. This isn’t rare. It’s a well-documented problem that affects thousands every year, especially when potent creams are used on the face, armpits, or groin-and often without proper guidance.
How Topical Steroids Thin Your Skin
Topical corticosteroids work by calming inflammation, but they don’t just target the bad cells. They also slow down the natural repair system in your skin. Keratinocytes-the cells that build the outer layer-and fibroblasts-the cells that make collagen-get suppressed. Collagen is what keeps your skin firm and elastic. When its production drops, your skin starts to lose structure. This isn’t just surface-level thinning. The deeper layers, including the dermis, shrink. The result? Skin that looks translucent, feels fragile, and tears easily.
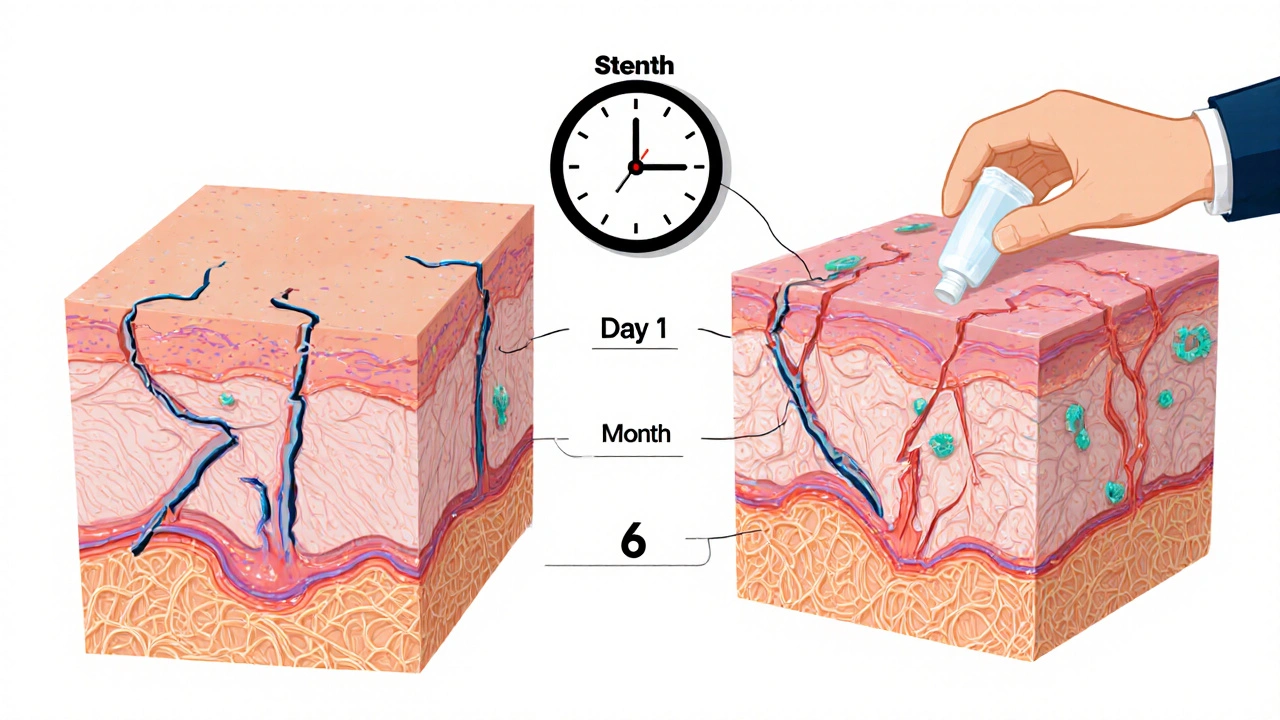
One of the first signs isn’t always visible. Before your skin looks thin, it starts leaking moisture. The barrier that holds in water and blocks germs breaks down because corticosteroids reduce ceramides, cholesterol, and fatty acids-the exact building blocks your skin needs to stay protected. This leads to increased transepidermal water loss, or TEWL. Your skin dries out, cracks, and becomes more open to bacteria and fungi.
Studies show that even three days of using a high-potency steroid can change how your skin functions. The damage might not be obvious yet, but the repair process is already slowed. By week two, the stratum corneum-the outermost protective layer-starts to thin. After months, you might notice fine lines turning into deep wrinkles, often called "elephant wrinkles" by patients. These aren’t aging lines. They’re structural collapse.
Who’s Most at Risk?
Not everyone gets skin atrophy the same way. Risk goes up with three things: potency, area, and duration.
Class I to IV corticosteroids (like clobetasol or betamethasone) are the strongest. They’re powerful-but also dangerous if used long-term. Class V to VII (like hydrocortisone 1%) are much safer for daily use. Yet many people buy stronger creams over the counter or get them prescribed for months without warning.
Thin skin areas are especially vulnerable. The face, eyelids, neck, armpits, groin, and inner thighs have less fat and fewer oil glands. Children’s skin is even thinner-up to five times more sensitive than adult skin. That’s why pediatricians warn against using strong steroids on babies, even for eczema.
Large surface area use is another red flag. Applying a potent steroid over half your body, even once a day, can lead to systemic absorption. That’s not just skin damage-it can affect your adrenal glands, blood sugar, and bone density too.
What Happens When Infections Set In
Thinned skin doesn’t just look different-it becomes an open door for germs. Fungal infections like candidiasis are common. You’ll see red, scaly patches with tiny pustules around the edges, often mistaken for a flare-up of eczema. That’s when people apply more steroid-and make it worse.
Bacterial infections follow. Staphylococcus aureus thrives in compromised skin. You might get impetigo-yellow crusting, oozing sores-or folliculitis-red bumps around hair follicles. These don’t respond to steroids. They need antibiotics. But if you keep using the cream, the infection hides under the redness and gets worse.
Then there’s perioral dermatitis. It looks like acne around the mouth, but it’s not acne. It’s a reaction to steroids applied to the face. It flares up when you stop using the cream, but it doesn’t go away until you stop completely. Many patients use steroids for months thinking it’s acne, only to end up with a chronic, burning rash.
The Withdrawal Trap
Stopping a steroid cream after long-term use isn’t simple. Your skin doesn’t bounce back overnight. In fact, it often gets worse before it gets better.
This is called Topical Steroid Withdrawal (TSW). It starts about a week after you quit. The skin turns bright red, burns, and itches-sometimes worse than before you started. You might feel like you’re on fire. This isn’t in your head. It’s a rebound inflammation. Your skin’s immune system, suppressed for so long, goes into overdrive.
Studies tracking 127 patients found that each flare after stopping gets shorter, but the recovery periods get longer. If you used steroids for six months, withdrawal might last four to six months. If you used them for years, recovery can take over a year. Reddit communities like r/eczema and r/SteroidAddiction have thousands of posts describing "burning face syndrome," peeling skin, and hair loss. The average recovery time reported by 891 users between 2020 and 2023 was 8.2 months.
And here’s the hard truth: there’s no magic cure. No cream, supplement, or diet fixes TSW. The only path is time-and careful support.
How to Prevent and Reverse the Damage
Prevention starts with using the weakest steroid that works. Don’t reach for clobetasol unless your dermatologist says so. Use it only for 5-7 days, never longer. Apply it once or twice a day-never more. Avoid using it on the face unless it’s a low-potency version, and even then, limit it to a few days.
If you’ve already got thinning skin, stop the steroid. But don’t quit cold turkey if you’ve been using it for more than two weeks. Taper slowly. For example, switch from a Class IV to a Class VI, then to a non-steroid moisturizer over 2-4 weeks. This reduces the shock to your skin.
Repair the barrier. Use a moisturizer with ceramides, cholesterol, and free fatty acids in a 3:1:1 ratio. This mimics your skin’s natural lipids. One 2020 trial showed this combo improved barrier function by 68.4% in eight weeks. Look for brands that list these exact ingredients-not just "ceramide" as a buzzword.
Protect your skin from the sun. UV rays break down collagen faster. In atrophic skin, sun damage multiplies. Use SPF 50+ every day-even if it’s cloudy. A 2004 study showed SPF 50+ reduced collagen loss by 42% in damaged skin areas.
Watch for infection signs: sudden redness, pus, crusting, or worsening burning. See a dermatologist. Don’t treat it yourself. You need antifungal or antibiotic treatment-not more steroid.

What’s Changing in the Medical World
Regulators are catching up. The FDA required "atrophogenic potential" warnings on all topical steroid packaging in 2010. The EMA followed in 2015. The UK’s MHRA issued specific guidelines in January 2022 for both prescription and over-the-counter products.
But sales are still rising. In 2023, $12.7 billion worth of topical steroids were sold worldwide. In the U.S. alone, 78 million prescriptions were written. Many are for eczema, psoriasis, and dermatitis-conditions that need long-term management. That’s why new alternatives are being developed.
Researchers are testing "dual-soft" glucocorticoid agonists that reduce inflammation without suppressing collagen. Early lab results are promising. The NIH is running a Phase II trial (NCT04567892) using a low-dose steroid combined with fibroblast growth factor to rebuild skin structure. Early data shows a 63% drop in atrophy compared to standard treatment.
The market for steroid-sparing treatments is expected to grow from $1.2 billion in 2023 to $3.8 billion by 2028. That’s not just business-it’s a sign that the medical community is finally listening to patients who’ve suffered long-term damage.
What You Can Do Today
If you’re using a topical steroid:
- Check the potency. Is it Class I-IV? If yes, ask your doctor if you really need it.
- How long have you been using it? If more than 2 weeks, talk to your doctor about tapering.
- Are you using it on your face? If so, switch to a low-potency version or non-steroid alternative.
- Is your skin burning, peeling, or breaking out? That’s not normal. Get it checked.
- Start using a ceramide-based moisturizer daily-even if you’re not done with the steroid.
Skin atrophy and steroid-related infections aren’t inevitable. They’re preventable. But they require awareness, caution, and sometimes, the courage to stop using something that felt like a miracle cure.
Can skin atrophy from topical steroids be reversed?
Yes, but only if caught early. Mild thinning from short-term use can improve over months with proper barrier repair and no further steroid use. Once striae (stretch marks) or deep wrinkles form, the damage is permanent because collagen fibers are broken. The skin can regain some thickness and strength, but not its original structure.
How long does it take for skin to recover after stopping steroids?
Recovery varies. For short-term use (under 4 weeks), skin may heal in 2-6 months. For long-term use (6+ months), withdrawal can last 12-24 months. The more you used and the stronger the steroid, the longer it takes. Patience and consistent barrier repair are key.
Are over-the-counter hydrocortisone creams safe for long-term use?
Hydrocortisone 1% is low potency and generally safe for short-term use (up to 2 weeks). But using it daily for months-even on a small patch-can still cause thinning, especially on the face or folds of skin. It’s not risk-free. Always use the lowest dose for the shortest time possible.
Can topical steroids cause infections even if you don’t see any symptoms?
Yes. Steroids suppress immune activity in the skin, letting fungi and bacteria grow unnoticed. You might not see redness or pus at first, but a skin biopsy or swab test can reveal hidden infections. That’s why persistent rashes that don’t respond to steroids should be evaluated by a dermatologist.
What are the safest alternatives to topical steroids for eczema?
Topical calcineurin inhibitors like tacrolimus and pimecrolimus are steroid-free options approved for eczema. Crisaborole is another non-steroid option. For maintenance, daily moisturizing with ceramide-rich creams, wet wrap therapy, and avoiding triggers like harsh soaps and heat can control flare-ups without steroids. Newer biologics like dupilumab are also effective for moderate to severe cases.
Should I avoid topical steroids completely?
No. They’re still essential for controlling severe inflammation in conditions like eczema, psoriasis, and contact dermatitis. The goal isn’t to avoid them-it’s to use them wisely: the lowest strength, shortest time, smallest area. When used correctly, their benefits far outweigh the risks.
If you’ve been using steroids for a long time and your skin feels thin, fragile, or constantly irritated, you’re not alone. The good news? Recovery is possible-with the right approach, patience, and support.


Matthew King
October 28, 2025 AT 19:17bro i used clobetasol on my face for two weeks thinking it was acne and now my skin looks like parchment paper. it’s been 8 months and i still burn in the sun. no joke, i wear a hat indoors now.
Rika Nokashi
October 29, 2025 AT 03:49It is utterly irresponsible, frankly, how easily accessible these Class I and II corticosteroids are-over the counter, even in pharmacies without a prescription-and yet the medical literature has been screaming about dermal atrophy for decades. The skin is not a surface to be masked; it is a dynamic, living organ system that communicates distress through microstructural collapse, ceramide depletion, and barrier dysfunction-none of which are reversible once collagen scaffolding is permanently degraded. You cannot ‘heal’ a broken dermal matrix with moisturizers alone. The damage is structural, and time, while necessary, is not sufficient without rigorous, evidence-based reconstruction protocols.
Joe Puleo
October 30, 2025 AT 05:19if you're using steroid cream for more than a week, talk to your doc. period. i used to think hydrocortisone was harmless-turns out i was wrong. switched to ceramide cream and my eczema actually got better. no burning, no peeling. just skin being skin again.
Meredith Poley
October 30, 2025 AT 08:11Oh wow, so now we’re blaming the medicine instead of people who treat their skin like a science experiment? I’m sure the FDA didn’t approve these for fun. If you’re using clobetasol like it’s hand lotion, don’t blame the drug-blame the idiot holding the tube.
Don Moore
October 31, 2025 AT 07:40Thank you for this comprehensive and clinically grounded overview. The emphasis on barrier repair with a 3:1:1 lipid ratio is particularly critical. Clinical trials consistently demonstrate that ceramide-dominant formulations restore transepidermal water loss metrics significantly faster than emollient-only products. For patients in withdrawal, a structured, multidisciplinary approach-dermatology, psychology, and nutrition-is the gold standard. Recovery is not linear, but it is possible with persistence and professional guidance.
Bhanu pratap
October 31, 2025 AT 16:45My cousin in Delhi used steroid cream for her baby’s rash for 6 months. The child’s skin turned transparent. She cried every night. Now she uses coconut oil and neem paste. No doctor. No pharmacy. Just love and tradition. The West overmedicates everything. Sometimes, less is more.
Andrea Swick
October 31, 2025 AT 21:20I didn’t realize how much I’d been masking my eczema until I stopped. The first week was hell-red, raw, burning like I’d been dipped in acid. But by month three, the skin started to breathe again. I stopped reaching for the cream. I started reaching for my moisturizer. And slowly, the cracks healed. It’s not glamorous. But it’s real.
Ben Jackson
November 1, 2025 AT 19:25Let’s not forget the systemic risks. Topical steroids aren’t just skin-deep-they can suppress the HPA axis, especially with large-area use. I’ve seen patients with adrenal insufficiency because they thought ‘it’s just cream.’ The FDA warning labels? Too little, too late. We need public health campaigns-not just packaging fine print.
Ikenga Uzoamaka
November 3, 2025 AT 03:55This is why we need to stop trusting Western medicine! I used a paste made from turmeric, honey, and aloe vera from my village-and my rash vanished in 3 days! Why pay for chemicals when nature gives us everything? The pharmaceutical companies don’t want you to know this!
Keith Bloom
November 3, 2025 AT 21:30you people are so gullible. steroid withdrawal? lol. it’s just your skin being dramatic. if you stop using it and your skin gets worse, maybe you were addicted to the feeling of relief, not the cream. also, ‘ceramide moisturizer’? that’s just fancy lotion with a $20 price tag. i used vaseline and lived.
Austin Levine
November 5, 2025 AT 19:45Has anyone tried the NIH’s dual-soft glucocorticoid trial? I read the early data-63% less atrophy. That’s huge. If this works, it could change everything.
Mathias Matengu Mabuta
November 6, 2025 AT 18:23Let us not ignore the geopolitical context: the $12.7 billion global steroid market is a direct consequence of neoliberal pharmaceutical hegemony. The FDA’s 2010 labeling requirement was a performative gesture to appease public outrage while allowing continued profit extraction from chronic disease management. The real solution lies not in ‘ceramides’ or ‘barrier repair,’ but in dismantling the medical-industrial complex that commodifies skin integrity as a product to be sold back to us.
Melissa Thompson
November 7, 2025 AT 10:12And yet, in America, we still have people using steroid creams on their toddlers because they’re too lazy to find a real dermatologist. In Germany, you need a prescription for hydrocortisone above 0.5%. In Japan, they use traditional herbal balms. We’re behind. We’re lazy. We’re addicted to quick fixes. And now our skin is paying the price.
Lee Lee
November 8, 2025 AT 10:21Did you know that the ‘steroid withdrawal’ phenomenon is a myth created by Big Pharma to sell ‘non-steroid’ alternatives? The burning, peeling, hair loss-all psychosomatic. The real issue is anxiety about stopping medication. The skin doesn’t ‘rebound.’ It’s your mind that’s rebelling. And the ‘ceramide’ trend? That’s just a rebrand of Vaseline with a fancy label. They’re milking trauma.
Amelia Wigton
November 10, 2025 AT 10:03It's worth noting, however, that the pathophysiological cascade initiated by topical corticosteroid exposure involves downregulation of the glucocorticoid receptor alpha isoform, leading to transcriptional suppression of key structural proteins-including filaggrin, loricrin, and involucrin-thereby compromising cornified envelope formation. Concurrently, MMP-1 and MMP-9 upregulation accelerates collagen degradation, which, once initiated, may not be fully reversible without fibroblast stimulation. Therefore, while barrier repair is critical, it is insufficient without concurrent modulation of the extracellular matrix. The NIH trial (NCT04567892) is promising precisely because it targets both inflammation and structural regeneration simultaneously.