Switching from a brand-name drug to a generic version is supposed to save money without sacrificing results. But for some people, it doesn’t work that way. You might feel different after the switch - more tired, more anxious, or worse, your condition might start to flare up. If you’ve been told your generic pill is "just as good," but you’re not feeling it, you’re not alone. The truth is, not all generics are created equal, especially when it comes to drugs where even small changes in dosage can cause big problems.
Why Some People Notice a Difference After Switching
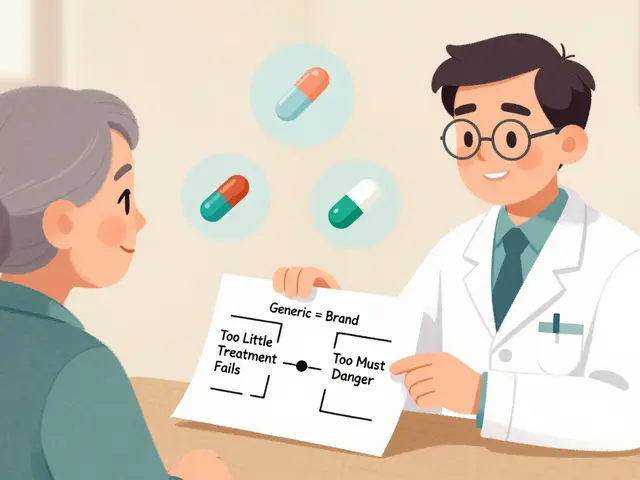
The FDA says generics must be bioequivalent to brand-name drugs. That means the amount of active ingredient in your blood should be within 80% to 125% of the brand. Sounds tight, right? But here’s the catch: that range allows for a 44% difference in total drug exposure between the two versions. For most medications, that’s fine. For others - especially those with a narrow therapeutic index (NTI) - it’s risky. NTI drugs are the ones where the difference between a helpful dose and a dangerous one is tiny. Think warfarin (blood thinner), levothyroxine (thyroid hormone), seizure meds like phenytoin, and digoxin (heart medication). A small change in how your body absorbs the drug can mean the difference between control and crisis. Studies show that after switching to generic levothyroxine, over 23% of patients had thyroid hormone levels that went out of range within six months. For warfarin, nearly 28% needed a dose adjustment within two months after switching. Even if the active ingredient is identical, the fillers, dyes, and coatings can vary. These inactive ingredients don’t treat your condition, but they can affect how fast the pill breaks down in your stomach. For someone with a sensitive gut, a different coating might mean the drug doesn’t absorb properly - or worse, causes nausea or diarrhea that makes them stop taking it.What to Track After a Generic Switch
You can’t just wait and hope things work out. You need to monitor your response. Here’s what matters most, broken down by type of medication:- For NTI drugs (warfarin, levothyroxine, digoxin, epilepsy meds): Lab tests are non-negotiable. Get your INR checked weekly for the first month after switching warfarin. For levothyroxine, check TSH levels at 4 and 8 weeks. For seizure meds, keep a daily log of seizure frequency and severity.
- For blood pressure or diabetes meds: Track your numbers at home. If your systolic BP jumps by 15+ points or your HbA1c rises by 0.5% or more in 60 days, that’s a red flag.
- For antidepressants or antipsychotics: Pay attention to mood, sleep, energy, and side effects like tremors or weight gain. If you feel worse after the switch - even if you can’t explain why - it’s worth reporting.
- For all medications: Note if you’ve stopped taking the drug entirely. A gap of 90 days or more in refills is a strong signal that something went wrong - either the drug didn’t work, or you couldn’t tolerate it.
How Healthcare Providers Should Be Helping
Doctors and pharmacists aren’t always trained to follow up after a switch. But the best practices are clear. According to the Institute for Safe Medication Practices, a good tracking plan has four phases:- Before the switch: Record your baseline. What were your last lab results? How often did you have symptoms? Write it down.
- Days 1-7: Get a call or message from your pharmacist. They should explain what to watch for and how to contact someone if things go wrong.
- Days 8-90: Schedule check-ins. For NTI drugs, weekly labs. For others, monthly check-ins or home monitoring logs.
- After 90 days: If everything’s stable, you can return to normal monitoring. If not, it’s time to reconsider the switch.

When You Should Ask to Go Back to the Brand
If you’ve been switched and you’re struggling, you don’t have to accept it. You have the right to ask for the brand-name drug again. But you need to make your case with data. Start with your records:- Lab results before and after the switch
- Symptom logs (seizures, panic attacks, fatigue levels)
- Any hospital visits or ER trips since the switch
What’s Changing in 2025
The system is starting to catch up. The FDA now requires post-market studies for all new NTI generics approved after January 1, 2024. That means manufacturers have to prove their product works in real patients - not just in lab tests. EHR systems like Epic are now flagging risky switches automatically. If you’re on warfarin and your INR drops 15% after a generic switch, your doctor gets a pop-up alert. In 2025, the FDA will launch a mobile app that lets patients report side effects or loss of effectiveness directly to the agency - no doctor visit needed. And AI tools are being tested to predict who’s most at risk. One study used 17 patient factors - age, kidney function, other meds, even how often they refill prescriptions - to guess who’d have trouble after a switch. It was 84% accurate.
What You Can Do Right Now
You don’t need to wait for the system to fix itself. Here’s your action plan:- Check your pill. Is the name on the label different from what you used to take? Write it down.
- Ask your pharmacist: "Is this the same as the brand?" and "Should I expect any changes?"
- Start a simple log: date, medication, dose, how you felt, any side effects.
- Set a reminder: 30 days after the switch, check your last lab result. Compare it to your pre-switch number.
- If anything feels off - even a little - don’t ignore it. Call your doctor. Bring your log.
Why This Matters Beyond Cost
Generic drugs are vital. They save the healthcare system billions. But cost savings shouldn’t come at the cost of safety. The goal isn’t to stop generics - it’s to make sure they work for everyone. When tracking is done right - with labs, logs, and follow-ups - success rates are high. One study of over 15,000 patients found that 96% stayed stable when pharmacists called them at 7, 30, and 90 days after a switch. That’s the difference between a system that just swaps pills - and one that actually cares about your health.Can I be forced to take a generic drug?
No. While many states allow pharmacists to substitute generics automatically, you have the right to refuse. You can ask for the brand-name drug by name at the pharmacy. Some insurance plans require prior authorization for brand drugs, but if your doctor writes "dispense as written" or "do not substitute" on the prescription, the pharmacy must honor it.
Are all generics the same?
No. Different manufacturers make the same generic drug, and they can use different fillers, binders, or coatings. These differences can affect how quickly the drug is absorbed. For most medications, it doesn’t matter. For narrow therapeutic index drugs, it can. That’s why switching between different generic brands - even if they’re both labeled the same - can sometimes cause problems.
How do I know if my drug has a narrow therapeutic index?
Common NTI drugs include warfarin, levothyroxine, digoxin, phenytoin, carbamazepine, cyclosporine, and lithium. Your doctor or pharmacist can tell you if your medication falls into this category. The FDA Orange Book also lists therapeutic equivalence codes - drugs marked "BX" are flagged as having potential bioequivalence concerns.
Should I track my symptoms even if I feel fine?
Yes. Some changes are subtle. You might not notice you’re more tired, or your anxiety is slightly worse - until it builds up. Tracking helps catch small shifts before they become big problems. Even if you feel fine, check your lab values if you’re on an NTI drug. A small change in blood levels can mean a big change in how you feel.
What if my doctor says the generic is fine, but I still don’t feel right?
Trust your body. Doctors rely on data, but you live with your symptoms. Bring your log, your lab results, and your concerns. Say: "I understand it’s supposed to be the same, but I’m not feeling the same. Can we try going back to the brand to see if it helps?" Many patients get better results when they advocate for themselves with evidence.


Chrisna Bronkhorst
November 10, 2025 AT 17:57The FDA’s 80-125% bioequivalence range is a joke. That’s not medicine, that’s a casino. I’ve seen patients on warfarin go from rock-solid INRs to nearly bleeding out after a generic switch. No one talks about the real cost: ER visits, hospitalizations, lost wages. The system is designed to save pennies while risking lives.
And don’t get me started on how pharmacies swap generics without telling you. I found out my levothyroxine changed because my TSH spiked - and the pharmacist had no idea I even noticed.
This isn’t about being picky. It’s about survival.
Amie Wilde
November 11, 2025 AT 20:00My mom switched to generic levothyroxine and got so tired she stopped driving. Took 3 months and 3 different generics before they figured out the brand was the only one that worked. Docs don’t listen until you’re in crisis.
Track everything. Even if you feel fine.
Gary Hattis
November 12, 2025 AT 11:24As someone who’s lived in 7 countries and taken meds in 5 different languages, I can tell you - the pill doesn’t care where it’s made. But your body does.
Here’s the thing: generics aren’t bad. Bad tracking is. In Brazil, they monitor TSH after every switch. In the US? You get a pill and a shrug.
It’s not the generic. It’s the system that doesn’t care enough to follow up. The Kaiser model proves it’s fixable. Why aren’t we doing it everywhere?
Esperanza Decor
November 12, 2025 AT 16:04I started logging my mood and sleep after my antidepressant switched. Within two weeks, I noticed I was waking up at 3 AM every day - no reason, no stress. My doctor dismissed it as ‘just stress.’ I brought the log. We switched back. I slept for 7 hours straight for the first time in a year.
Don’t let anyone tell you your experience isn’t valid. Your body remembers. Write it down. Show up with data. You’re not overreacting - you’re doing the work they’re paid to do.
Deepa Lakshminarasimhan
November 14, 2025 AT 02:19Did you know the same generic can come from different factories? One batch is made in India, another in China. The fillers change. The coating changes. The FDA doesn’t test every batch. They test one per year.
And the companies? They know this. That’s why they make generics cheaper - they cut corners. The ‘same drug’ is a lie. They’re selling placebo-grade versions and calling it science.
Next time you see a generic label, ask: who’s really behind this? And why are they allowed to gamble with your life?
Erica Cruz
November 15, 2025 AT 12:38Oh wow, another ‘I feel different’ post. Newsflash: placebo effect is real. You think your anxiety is from the pill? It’s from the fear of switching. I’ve seen this 200 times. People panic, then blame the generic.
And now we’re going to spend billions on ‘tracking logs’ and ‘AI predictors’ because someone can’t handle a pill that looks different?
Get a grip. Most people are fine. The outliers aren’t victims - they’re attention-seekers with confirmation bias.
Johnson Abraham
November 15, 2025 AT 14:34generic = bad? lol. i took generic xanax for 5 yrs. no prob. my buddy took brand. same thing. why u always think ur special? ur body dont magic.
also why u got a log? r u a robot? just take the damn pill.
ps: my dog took my meds once. still alive. so chill.
:P
Shante Ajadeen
November 16, 2025 AT 08:30I’m a nurse and I’ve seen this too many times. A patient comes in with a TSH of 12 after switching generics. They’re exhausted, depressed, gaining weight. We switch them back - TSH drops to 2.5 in 3 weeks.
It’s not about being difficult. It’s about listening. Your doctor isn’t a bad person - they’re just overloaded. Bring your log. Be calm. Be clear. You’re not asking for special treatment. You’re asking for basic care.
And if they say no? Ask for a pharmacist consult. Most hospitals have them now. They’re your secret weapon.
dace yates
November 17, 2025 AT 23:14How do you know which generic you’re getting? Is there a way to check the manufacturer code on the pill? I’ve never seen that info on the bottle.
Danae Miley
November 19, 2025 AT 04:15Correction: the FDA’s bioequivalence range is 80–125% for AUC and Cmax, not ‘total drug exposure.’ The original post misrepresents the data. Also, the 23% levothyroxine instability figure comes from a single 2017 observational study - not a meta-analysis. Precision matters when discussing clinical outcomes.
That said, the core message is valid: NTI drugs require vigilance. And pharmacists should be required to document substitutions. This isn’t about fear - it’s about accountability.