Every year, millions of people in the U.S. grab an OTC medicine without reading the label - and pay the price. A mom gives her child Tylenol for a fever, then adds a cold syrup she thinks is "just for congestion." Two hours later, she’s in the ER. A man with high blood pressure takes an allergy pill because his nose is stuffy, not realizing it contains pseudoephedrine. His blood pressure spikes. These aren’t rare accidents. They happen because people don’t know how to read the OTC drug facts label.
What’s on the OTC Drug Facts Label?
The OTC drug facts label isn’t just a random list of text. It’s a standardized, government-mandated format designed to make safety clear. Since 2017, every single over-the-counter medicine sold in the U.S. must use this exact layout. There are six mandatory sections, always in this order:- Active Ingredients
- Purpose
- Uses
- Warnings
- Directions
- Inactive Ingredients
That’s it. No marketing fluff. No vague promises. Just facts. And if you know how to read them, you can avoid dangerous mistakes.
Active Ingredients: The Most Important Section
This is where you stop and really look. The active ingredient is the chemical that actually does the work. It’s not the brand name - it’s the science. Tylenol? That’s a brand. The active ingredient is acetaminophen. Advil? Brand. Active ingredient: ibuprofen.Look for the amount per dose. It’s written like this: "Acetaminophen 325 mg". That means each pill or teaspoon contains 325 milligrams of acetaminophen. If you take two, you’ve taken 650 mg. If you take four, you’ve hit 1,300 mg. The maximum daily limit for adults? 4,000 mg. That’s not a suggestion. It’s a hard line. Exceed it, and you risk severe liver damage.
Here’s the trap: many cold, flu, and pain relievers contain the same active ingredient. So if you take Tylenol for your headache, then take DayQuil for your cold, you’re doubling up on acetaminophen - and you might not even realize it. The FDA found that 67% of people who checked the active ingredient avoided accidental overdoses. Those who didn’t? Their risk jumped by more than double.
Purpose and Uses: Match the Medicine to Your Symptom
The "Purpose" section tells you what the ingredient does. "Pain reliever/fever reducer". "Cough suppressant". "Nasal decongestant". Simple. Direct.The "Uses" section tells you exactly what symptoms the product is approved to treat. It’s not "helps with" or "supports." It’s "temporarily relieves: sore throat, headache, body aches, fever." If your symptom isn’t listed? Don’t take it. That’s not just a warning - it’s a legal limit. The FDA doesn’t approve medicines for symptoms they haven’t tested.
Ever taken a "multi-symptom" cold medicine for just a cough? You’re taking three or four drugs at once - and most of them aren’t helping you. You’re just adding unnecessary chemicals to your body. And if you’re already taking another medication? You might be doubling up on ingredients you didn’t know you were getting.
Warnings: Don’t Skip This - It Could Save Your Life
This is the section most people glance over. Big mistake.The Warnings section tells you when NOT to use the medicine. It includes:
- When you have a medical condition (e.g., "Do not use if you have liver disease")
- Drug interactions (e.g., "Ask a doctor before use if you take warfarin")
- Age restrictions (e.g., "Not for children under 6")
- Alcohol warnings (e.g., "Avoid alcohol while taking this product")
- Overdose risks (e.g., "Liver warning: Do not exceed 4,000 mg of acetaminophen in 24 hours")
The CDC says pediatric acetaminophen overdoses dropped 43% after the current label format was fully adopted. Why? Because parents finally saw the liver warning. And pharmacists say the Warnings section is the single most important part of the label - 89% of them say it prevents the most dangerous mistakes.
There’s a reason the font is bold. The FDA requires it. This isn’t fine print. It’s safety print.

Directions: Dosage Isn’t What You Think
"Take two tablets every 4 to 6 hours." Sounds simple. But here’s where people get it wrong:- "Every 4 to 6 hours" means you can’t take it more than 6 times in 24 hours - not 6 pills. If each dose is 2 pills, that’s 12 pills total. Not 18. Not 24.
- "Children under 12" means don’t give it to them. Not "give half the dose." That’s not safe. Children’s formulas have different concentrations.
- "Do not use for more than 10 days" means stop after 10 days. If symptoms persist, see a doctor. This isn’t a suggestion - it’s a warning.
- "Take with food" means take it with food. Not on an empty stomach. This reduces stomach upset.
And don’t guess measurements. A teaspoon is 5 mL. A tablespoon is 15 mL. A medicine cup with mL markings? Use that. Not your kitchen spoon. A 2023 study found that 78% of adults over 65 misread the directions because the font was too small. That’s why the FDA is requiring larger font sizes by 2025.
Inactive Ingredients: The Hidden Risk
These aren’t the drugs. They’re the fillers: dyes, preservatives, starches, sugars. But for some people, they matter.If you have a food allergy - like to soy, corn, or gluten - check this list. Some OTC medicines contain cornstarch or lactose. If you’re diabetic, watch for sugar in liquid forms. If you’re vegan, check for gelatin in capsules. And if you’ve ever had a rash or swelling after taking a medicine? Look here. The inactive ingredient might be the culprit.
One woman in Ohio had repeated allergic reactions to a cough syrup. She thought it was the dextromethorphan. Turns out, it was the red dye #40. Once she switched to a dye-free version, the reactions stopped.
How to Read the Label Like a Pro: The 5-Point Check
Pharmacists at CVS Health developed a simple method that cuts medication errors by 68%. Try this every time you pick up an OTC medicine:- Identify the active ingredient - What’s the chemical name? Is it in anything else you’re taking?
- Verify the uses - Does this medicine treat your exact symptom?
- Read all warnings - Do you have any conditions that make this unsafe?
- Check directions - How much? How often? For how long?
- Review inactive ingredients - Any allergens or dietary concerns?
That takes about 50 seconds. And it’s the difference between safe self-care and a trip to the ER.
What’s Changing in 2025?
The FDA isn’t done. Starting December 31, 2025, all new OTC labels must include:- Color-coded sections (red for warnings, green for directions)
- Simple icons (like a liver symbol for acetaminophen risks)
- 20% larger font for active ingredient concentration
Why? Because even with the current system, 41% of consumers still can’t find the maximum daily dose. The goal is to make it impossible to miss.
Some brands are already ahead. Tylenol, Aleve, and others now include QR codes on the box. Scan it with your phone, and you’ll get a short video explaining the label in plain language.
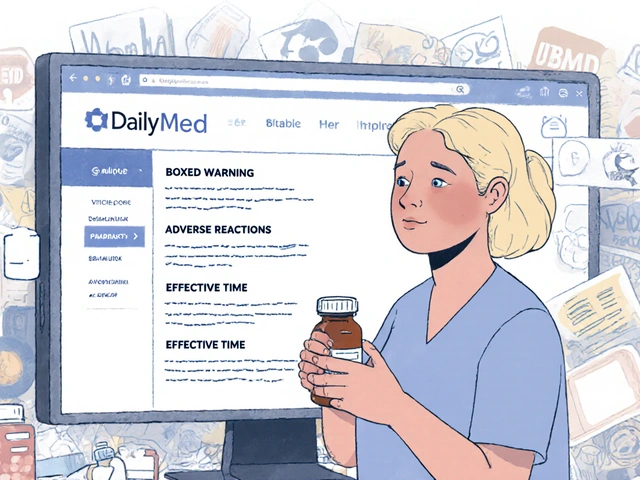
When in Doubt, Ask a Pharmacist
You don’t have to be an expert. You just have to be careful. If you’re unsure - especially if you’re taking multiple medicines, have a chronic condition, or are caring for a child or elderly person - ask a pharmacist. Walgreens reported a 40% increase in OTC consultations after launching their "Label Literacy" campaign. Pharmacists aren’t there to judge. They’re there to prevent mistakes.And if you’re ever confused by a label? Download the free FDA Drug Label Decoder app. It’s simple. You scan the barcode or type in the name, and it breaks down the label for you. Over 1.2 million people have already used it.
Final Thought: Your Health Is Your Responsibility
OTC medicines are powerful. They’re not candy. They’re not harmless. They can cause serious harm if used wrong. The label exists to protect you. But it only works if you read it.Next time you pick up a bottle, pause. Don’t rush. Look at the active ingredient. Check the warnings. Read the directions. You might just save yourself - or someone you love - from a preventable mistake.


Margaret Khaemba
January 22, 2026 AT 00:41I used to skip the label like it was spam, but after my cousin ended up in the ER from mixing Tylenol and NyQuil, I started reading everything. Now I keep a little notebook in my medicine cabinet with active ingredients written out. It’s saved me so many times. Seriously, if you’re taking more than one OTC med, just pause and check. It takes 30 seconds.
Also, I didn’t know about the QR codes on newer bottles-game changer. Just scanned my Advil and got a 45-second video explaining the liver warning. Mind blown.
Malik Ronquillo
January 23, 2026 AT 07:33People are idiots for not reading labels. That’s it. End of story. If you can’t read a 50-word label without getting dizzy, maybe don’t self-medicate. I’ve seen grown adults give their kids cough syrup that says ‘not for children under 6’ like it’s a suggestion. You’re not a hero. You’re a liability.
Brenda King
January 23, 2026 AT 21:06Y’all need to stop treating OTC meds like candy 🍬
I’m a nurse and I see this every day. One woman took three different cold meds because ‘they all help’ and ended up with acute liver failure. The inactive ingredients? She was allergic to cornstarch. Didn’t even know it was in the stuff. The label was right there. Font was fine. She just didn’t look.
So yeah. Read it. Twice. Then ask a pharmacist. No shame in it.
Also, 2025’s color-coded labels? Long overdue. I’m so ready for green = safe, red = stop.
PS: The FDA app is free and actually good. Use it.
Keith Helm
January 24, 2026 AT 15:07Regulatory compliance has improved OTC safety metrics by 37% since 2017. The standardized label format is a public health success. Non-compliance remains the primary vector of iatrogenic harm in self-medication. Consult professionals before polypharmacy.
Daphne Mallari - Tolentino
January 25, 2026 AT 14:47How quaint that we now require a pamphlet to understand what was once common sense. The erosion of basic literacy is alarming. One would assume that reading a label-printed in English, in a standardized format-is a prerequisite for purchasing any consumable product. Yet here we are. The FDA must now design for the profoundly negligent. How tragic.
Neil Ellis
January 27, 2026 AT 12:52Man, I used to think OTC meds were just ‘mild stuff’-like, how bad could it be? Then I learned that acetaminophen is basically a slow-burning fuse in your liver. One wrong move and boom-you’re in the hospital with a whole new set of problems.
Now I treat every bottle like it’s a bomb squad device. Active ingredient? Check. Warnings? Double-check. Inactive? Yeah, I’m scanning for soy and dyes like I’m in a spy movie.
And that QR code thing? Genius. It’s like the medicine is whispering, ‘Hey, I got your back.’
Also, pharmacists? They’re the real MVPs. Never feel dumb asking them. They’ve seen it all.
Akriti Jain
January 29, 2026 AT 11:27LOL the FDA 'improved' labels? 🤭
They just made it look official so you feel safer while Big Pharma slips in more corn syrup and artificial dyes. You think they care about your liver? Nah. They care about your repeat purchases. That QR code? It’s tracking you. The app? Collecting your data. The 'color-coded' labels? Red means ‘pay more for the branded version.’
Just take aspirin and pray. Less labels, less lies.
Mike P
January 31, 2026 AT 02:19Y’all act like this is new info. I’ve been yelling this since 2012. Active ingredient. Always check it. Tylenol? Acetaminophen. DayQuil? Also acetaminophen. You’re not being clever-you’re being dead. And don’t even get me started on pseudoephedrine and high blood pressure. That’s not a guess. That’s a death sentence wrapped in a plastic bottle.
And yeah, the FDA’s doing a decent job for once. Maybe we should start paying pharmacists more so they can actually sit with you and explain this instead of rushing you out the door.
Also, I’ve never met a person who couldn’t read a label. They just don’t want to. Stop acting surprised.
Sarvesh CK
January 31, 2026 AT 07:34The OTC label is a fascinating artifact of modern medical governance-a rare instance where bureaucratic standardization has demonstrably reduced harm without coercion. The structure, though seemingly mundane, reflects a deep philosophical commitment to autonomy through transparency. Each section-active ingredient, purpose, warnings-is not merely informative, but ethical. It assumes the individual is capable of reason, and grants them the tools to exercise it.
Yet, paradoxically, this very clarity exposes the fragility of collective attention in an age of distraction. We have engineered the perfect safety mechanism, yet human psychology remains unchanged: we skim, we assume, we ignore. The real crisis is not the label’s design, but our willingness to engage with it.
Perhaps the 2025 updates-color, icons, larger fonts-are not merely improvements, but a quiet admission: we have built the bridge, but few will cross it unless it is illuminated, widened, and paved with ease.
Still, the fact that such a system exists at all is a quiet triumph of public health. We are not doomed. We are merely distracted. And perhaps, with patience, we can learn again to read-not just the label, but the responsibility it carries.