For millions of people with sleep apnea, the CPAP machine is a nightmare - not because it doesn’t work, but because it’s unbearable to wear night after night. The mask digs into your face, the hose tangles, the air pressure feels like choking, and the noise drives your partner crazy. If you’ve tried CPAP and walked away, you’re not alone. Nearly half of people stop using it within the first year. But there’s another option that doesn’t involve a mask, a hose, or nightly frustration: upper airway stimulation.
What Is Upper Airway Stimulation?
Upper airway stimulation (UAS) is a surgically implanted device that treats obstructive sleep apnea by gently stimulating the nerve that controls your tongue. It’s not a cure, but it keeps your airway open while you sleep without needing a mask. The most common system is called Inspire, developed by Inspire Medical Systems. It was approved by the FDA in 2014 and has since helped over 200,000 people worldwide.How does it work? While you sleep, the device senses when you inhale and sends a mild electrical pulse to the hypoglossal nerve. That nerve controls the muscles in your tongue. The pulse moves your tongue slightly forward, preventing it from collapsing backward and blocking your airway. It only activates during breathing - not all night - so there’s no constant stimulation or muscle fatigue.
How It’s Different from CPAP
CPAP works by blowing air through a mask to keep your throat open. It’s effective - but only if you wear it. Studies show 29% to 46% of people abandon CPAP within a year. The reasons? Discomfort, claustrophobia, dry mouth, skin sores, and noise. Many say it ruins their sleep more than the apnea itself.Upper airway stimulation solves the compliance problem. Once implanted, you don’t need to wear anything on your face. You just flip a small remote control on before bed and off when you wake up. No masks. No hoses. No noise. Patients report higher satisfaction: 86% say it’s better than CPAP, and 80% would recommend it to someone else.
Who Is a Good Candidate?
This isn’t for everyone. You need to meet specific medical criteria:- You have moderate to severe obstructive sleep apnea (AHI between 15 and 100 events per hour)
- Your BMI is under 35 (some centers accept up to 40)
- You’ve tried and failed CPAP - meaning you used it less than 4 hours a night for at least 30 days
- You don’t have mostly central apneas (those caused by your brain not signaling your body to breathe)
- Your airway isn’t completely collapsed when sedated - confirmed by a special endoscopy test
- You’re at least 22 years old
If you’re overweight, have severe nasal blockages, or have a lot of central apneas, UAS probably won’t help. It’s designed for people with anatomical obstruction - a tongue or soft tissue that falls back during sleep.
The Procedure: What to Expect
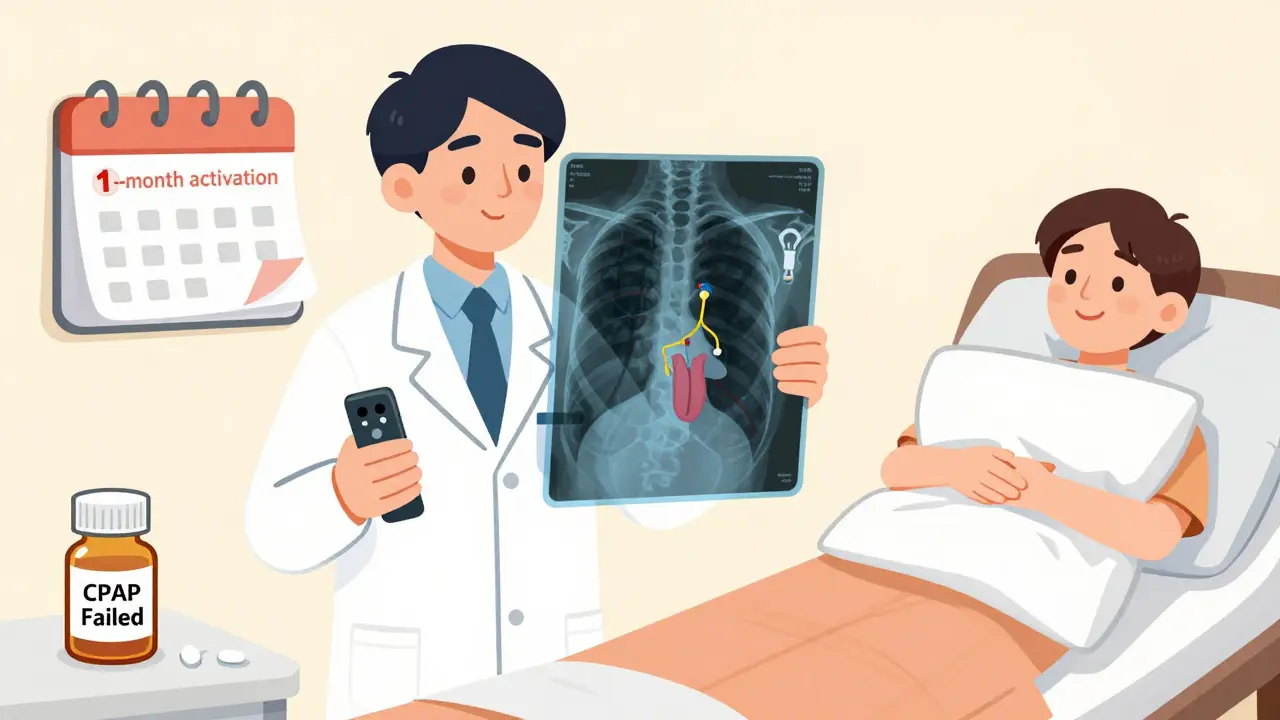
The surgery is done as an outpatient procedure under general anesthesia. Three small incisions are made: one in the neck to access the nerve, one lower in the neck to place a sensor near the windpipe, and one below the collarbone to implant the battery-powered pulse generator.The whole thing takes about 2 to 3 hours. Most people go home the same day. Recovery is quick: you’ll feel sore for a few days, but most return to normal activities within a week. There’s no overnight hospital stay.
Activation doesn’t happen right away. Your doctor waits about a month for healing. Then, during a short office visit, they turn on the device and adjust the stimulation level using a programming wand. You’ll get a remote control to turn it on and off each night.

How Effective Is It?
The data speaks for itself. In the landmark STAR trial, patients saw their apnea events drop from an average of 29 per hour to just 9 - a 68% reduction. Two-thirds of patients achieved at least a 50% improvement, and 80% ended up with an AHI under 20, which is considered mild or better.Long-term results are just as strong. A five-year follow-up study showed patients maintained those improvements. Daytime sleepiness dropped significantly. People reported feeling more alert, focused, and energetic. Bed partners noticed a huge difference: 85% said snoring stopped or became very quiet.
Complications are rare. Over 99% of patients had no major issues. The most common side effects are temporary tongue weakness (5% of cases) or minor swelling at the incision sites. Infection happens in about 2% of cases - similar to other implant surgeries. The device can be removed if needed, making it reversible, unlike most other sleep apnea surgeries.
Cost and Insurance
The total cost - including surgery, device, and follow-up - ranges from $35,000 to $40,000. That sounds steep, but it’s comparable to the long-term cost of CPAP when you factor in masks, tubing, repairs, and replacement machines every 5 years.Good news: insurance coverage has expanded dramatically. As of 2023, 95% of Medicare patients and 85% of privately insured patients have coverage for Inspire therapy. Most insurers require proof of CPAP failure before approving the implant. Your doctor’s office will usually handle the pre-authorization process.
Real Stories, Real Results
One patient in Manchester, who asked to remain anonymous, had used CPAP for six years. He wore it inconsistently and still woke up gasping. After getting the Inspire implant, he said: “I don’t remember the last time I woke up because I couldn’t breathe. My wife says I’m quiet now. I feel like I’m 10 years younger.”Another user on a sleep forum wrote: “I used to dread bedtime. Now I turn on the remote, roll over, and sleep. No mask. No noise. No guilt. I wish I’d done this five years ago.”
Not everyone has a perfect experience. Some report a strange tingling sensation at first - like a mild electric buzz in the tongue. It usually fades after a few weeks. Others forget to turn it on. That’s why the remote is so important. If you skip a night, your apnea returns.
How It Compares to Other Surgeries
Traditional surgeries for sleep apnea - like removing tonsils, shrinking the soft palate, or repositioning the jaw - are more invasive, painful, and unpredictable. Many require long recovery times and don’t guarantee results. UAS avoids cutting or removing tissue. It works by gently moving structures into place, not destroying them.Unlike jaw surgery, which can change your bite or facial appearance, UAS leaves your anatomy untouched. Unlike tongue reduction, it doesn’t risk permanent numbness or swallowing problems. It’s a targeted, reversible intervention that adapts to your breathing.
What’s Next for This Technology?
The FDA expanded eligibility in 2023 to include patients with higher BMI and more severe apnea. That means more people can now qualify. Researchers are working on smaller devices, longer battery life, and AI-powered systems that automatically adjust stimulation based on your sleep position or alcohol intake.One study is testing whether machine learning can predict who will respond best to UAS by analyzing airway scans. That could make patient selection even more accurate. As more doctors get trained in the procedure, access is improving. The global market for this therapy is expected to grow over 14% per year through 2028.
Is It Worth It?
If you’ve given up on CPAP and still struggle with daytime fatigue, loud snoring, or high blood pressure linked to sleep apnea, upper airway stimulation offers real hope. It’s not a magic fix - it requires surgery, a habit change, and ongoing care. But for those who qualify, it’s the most effective alternative to CPAP we have today.The benefits go beyond sleep. Better sleep means lower risk of stroke, heart disease, and diabetes. It improves mood, memory, and relationships. It can even help you stay alert while driving.
It’s not for everyone. But if you’ve tried everything else and still can’t breathe at night, this might be the answer you’ve been waiting for.
Is upper airway stimulation the same as a CPAP machine?
No. CPAP uses air pressure delivered through a mask to keep your airway open. Upper airway stimulation uses a small implant to stimulate a nerve that moves your tongue forward, preventing blockage. There’s no mask, no hose, and no air pressure involved.
How long does the device last?
The battery in the implant lasts about 11 years. When it runs out, the generator can be replaced in a simple outpatient procedure. The leads (wires) are designed to last much longer and rarely need replacement.
Can I have an MRI with the implant?
Yes - but only under specific conditions. The Inspire device is MRI-conditional. That means you can have an MRI of your head or neck, but not your chest or abdomen, and only if the device is turned off before the scan. Always inform your radiology team that you have an implanted device.
Will I feel the stimulation all the time?
No. The device only activates during inhalation while you’re asleep. During the day, you won’t feel anything. At night, you might feel a mild tingling or pulling sensation in your tongue - similar to a muscle twitch. Most people get used to it within a few weeks.
What if I forget to turn it on?
If you forget, your airway will collapse as it did before the implant, and apnea events will return. That’s why the remote is important. Some patients set a reminder on their phone. Others leave the remote on their nightstand next to their toothbrush. It becomes part of your bedtime routine, like brushing your teeth.
Can I travel with the device?
Absolutely. The remote is small and fits in your pocket. You can fly, drive, or stay in hotels without issues. Airport security won’t trigger alarms - the device is made of titanium and doesn’t contain metal strong enough to set off detectors. You’ll get a patient ID card from your doctor to show if asked.
Does it help with snoring?
Yes - and that’s one of the biggest benefits patients report. Since snoring is caused by airway obstruction, and UAS keeps the airway open, snoring drops dramatically. Studies show 85% of bed partners report no snoring or only soft snoring after four years of use.
How soon will I notice results?
Most people notice better sleep within the first week after activation. Daytime energy improvements usually show up in 2 to 4 weeks. Full results - like reduced blood pressure and improved cognitive function - take 3 to 6 months as your body adjusts to consistent, restful sleep.
Is this covered by insurance in the UK?
As of 2026, upper airway stimulation is not routinely funded by the NHS in the UK. It is available privately, and some private health insurers may cover it if CPAP has failed. Patients often travel to the U.S. or Europe for the procedure due to better coverage and availability. Check with your insurer for specific policy details.
Are there any long-term risks?
Long-term risks are very low. The device has been in use for over a decade, and data shows no increased risk of nerve damage, infection, or systemic issues. The most common long-term concern is battery replacement after about 11 years, which is a minor procedure. No cases of device-related death have been reported.


Kiran Plaha
January 5, 2026 AT 20:10I never knew this was an option. I tried CPAP for months and just gave up. My wife was sleeping in the guest room. This sounds like a miracle.
Kelly Beck
January 6, 2026 AT 04:57OMG I’ve been waiting for something like this for YEARS. My husband refused CPAP because he said it felt like he was being suffocated by a plastic ghost. He got the Inspire implant last year and now he snores less than me (and I don’t even have apnea). We’re both sleeping through the night for the first time in a decade. I cried when I heard his breathing was normal. Seriously, if you’re struggling with CPAP - don’t give up. This exists. It’s real. It works. 🥹💖
Isaac Jules
January 7, 2026 AT 05:34LMAO another $40k ‘solution’ for people who can’t follow basic medical advice. You think this is magic? It’s just a fancy pacemaker for your tongue. Meanwhile, people in developing countries are using nasal strips and sleeping on their side. Stop treating sleep apnea like a luxury car upgrade.
Amy Le
January 7, 2026 AT 21:21Of course it’s covered by insurance in the US - because we turn every medical problem into a corporate profit center. In India, they just tell you to lose weight and stop drinking. Guess which approach is cheaper? 😏
Harshit Kansal
January 8, 2026 AT 13:22My uncle got this done in Texas last year. He said the remote feels like a TV controller. He forgets to turn it on sometimes and wakes up gasping like a fish. But hey - at least he’s not wearing a mask anymore. We all laugh about it now. He calls it his ‘tongue zapper’.
Brian Anaz
January 9, 2026 AT 01:22Let’s be real - this is just another way for big med to milk Americans. You think your insurance is gonna cover this in 2030? Nah. They’ll make you pay $15k out of pocket and call it ‘premium care’. Meanwhile, the real solution is sleep hygiene. But who wants to go to bed early and stop eating pizza at midnight?
Pavan Vora
January 9, 2026 AT 19:46In India, we don't have this option, but we have our own wisdom - sleep on your side, avoid heavy meals before bed, and if you're overweight, lose weight. Simple. No surgery. No remote. No $40,000 bill. I’m not saying this is bad - I’m saying maybe we need to look at the root, not just the symptom.
Vinayak Naik
January 10, 2026 AT 19:27Bro this thing is straight-up sci-fi. I used to wake up like I’d been strangled by a ghost. Now I flip the remote like I’m turning on my PlayStation. My wife says I sound like a baby now. I didn’t think I’d ever sleep like a normal person again. Also, the battery lasts 11 years? That’s longer than my last phone. 😎
Katie Schoen
January 12, 2026 AT 11:31So… you’re telling me I can finally stop pretending I’m a cyborg with a snorkel on my face? Sign me up. I’ve spent more on CPAP masks than I have on my car. At least this thing doesn’t make me feel like I’m auditioning for a dystopian Netflix show.
Beth Templeton
January 12, 2026 AT 12:58It’s a device. Not a cure. Stop acting like it’s the second coming.
Venkataramanan Viswanathan
January 14, 2026 AT 12:17It is indeed a remarkable advancement in medical technology, yet one must not overlook the foundational importance of lifestyle modifications, such as weight management and positional therapy, which remain the most sustainable and universally accessible interventions for obstructive sleep apnea.
Indra Triawan
January 15, 2026 AT 22:43I just want someone to tell me it’s okay if I can’t afford this. I tried CPAP. I hated it. I cried every night. I feel like a failure because I can’t do the ‘right’ thing. Is my sleep not worth $40k? Do I just have to keep suffering because I’m not rich enough to sleep?
Saylor Frye
January 16, 2026 AT 02:58Wow, another Silicon Valley medical fantasy sold to the masses. You know what’s cheaper than a $40k tongue zapper? Sleeping on your side. Or not eating a whole pizza before bed. Or losing 20 pounds. But hey - why fix the problem when you can implant a gadget and charge insurance for it? This isn’t innovation. It’s capitalism with a pacemaker.
Molly McLane
January 17, 2026 AT 00:48To the person who said they feel like a failure because they can’t afford this - you’re not a failure. You’re human. This technology is incredible, but it’s not the only path to better sleep. Some of us make small changes - a wedge pillow, cutting out alcohol, sleeping on our side - and it makes a difference. You’re not broken. The system is just stacked. Keep trying. You deserve rest. And you’re not alone.