Every year, thousands of people in the UK and around the world accidentally take too much of a medication - not because they meant to, but because they lost track. A simple pill taken at the wrong time, a double dose mixed up with a similar-looking one, or combining painkillers with alcohol can turn a routine habit into a life-threatening mistake. The good news? You don’t need fancy tech or a doctor’s permission to stop this from happening. All you need is a medication log.
Why a Medication Log Matters More Than You Think
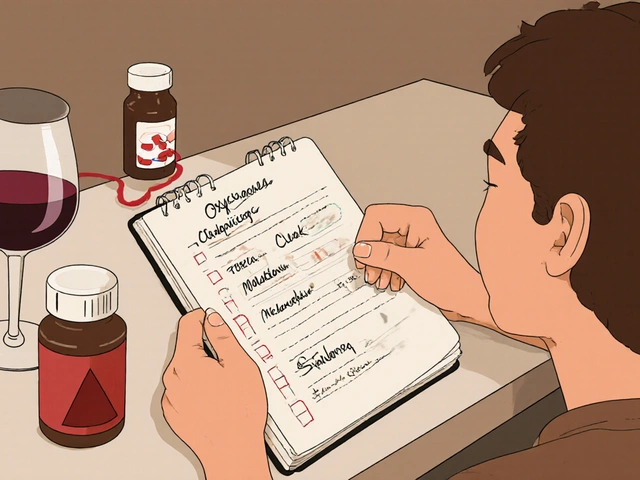
Most people think overdose only happens with illegal drugs or when someone takes too many pills on purpose. But the truth is, most overdose deaths involve prescription medications - especially opioids, benzodiazepines, and even common painkillers like acetaminophen. A 2023 CDC report showed that nearly 40% of opioid-related overdoses involved patients who were taking multiple medications without realizing the risks. A medication log isn’t just for people with addiction. It’s for anyone taking more than one drug, especially if they’re managing chronic pain, anxiety, sleep issues, or mental health conditions. It’s for older adults juggling five different prescriptions. It’s for people using over-the-counter meds alongside supplements. It’s for anyone who’s ever thought, “Wait, did I take that already?” The log works because it turns guesswork into facts. Instead of relying on memory - which is unreliable, especially under stress or fatigue - you have a written record of what you took, when, and how you felt. This isn’t just about avoiding overdose. It’s about knowing what’s working, what’s not, and when to speak up to your doctor.What to Write in Your Medication Log
A good log doesn’t need to be complicated. You’re not writing a novel. You’re recording key facts that can save your life. Here’s exactly what to include for every entry:- Medication name - Use the full name, not the brand. Write “oxycodone 5mg” not “Percocet.”
- Dosage - How many milligrams or pills? Write “1 tablet” or “20mg.” Don’t say “a little” or “a bit.”
- Time taken - Use a 24-hour clock. “14:30” is clearer than “2:30 PM.”
- Purpose - Why did you take it? “For back pain,” “for anxiety,” “for sleep.”
- Method of use - Swallowed? Crushed? Snorted? Injected? This matters. Taking a pill by mouth is far safer than crushing and snorting it - and your log should reflect that.
- Other substances taken - Alcohol? Benzodiazepines? Sleep aids? Even a glass of wine or a melatonin tablet can dangerously interact with opioids or sedatives.
- Effects or side effects - Did you feel drowsy? Nauseous? Clear-headed? Any unusual symptoms? This helps you spot patterns.
For example:
11/15/2025, 10:15 - Oxycodone 5mg, swallowed, for lower back pain. Took with a glass of water. No alcohol. Felt drowsy after 45 min. No nausea.
That’s it. Five lines. Takes less than a minute. But if you ever end up in the ER, that log could tell the staff exactly what you took - and what you didn’t - and help them treat you faster.
Choose Your Format: Paper or Digital?
You don’t need an app. A notebook works perfectly. But if you’re used to phones, a digital log might be easier to keep up with.Paper Log
Buy a small notebook - one that fits in your pocket or purse. Use a pen, not a pencil. Write the date at the top of each page. Keep it with you. If you’re traveling, take it. If you’re visiting your doctor, bring it. Paper doesn’t die. It doesn’t need charging. It’s always there.Digital Log
If you prefer apps, use something simple. Google Keep, Apple Notes, or even a plain text file on your phone works. Some pharmacy apps like MyTherapy or Medisafe let you track meds and send reminders. But don’t rely on them to alert you about interactions - most don’t check for dangerous combos like alcohol + opioids.Important: If you use a digital log, make sure someone you trust knows how to access it. In an emergency, your phone might be locked. Your loved ones need to know where to look.

How to Use Your Log to Avoid Overdose
Just writing things down isn’t enough. You have to use the log to make smarter choices.1. Start Low, Go Slow - and Record It
If you’re starting a new medication, or changing your dose, follow the rule: start low, go slow. The Substance Abuse and Mental Health Services Administration (SAMHSA) says this is one of the most effective ways to avoid overdose.Example: You’re prescribed oxycodone for the first time. The doctor says 5mg every 6 hours as needed. Don’t take two pills on day one just because the pain feels bad. Take one. Write it down. Wait. See how you feel. Did your pain go down? Did you feel dizzy? Sleepy? Nauseous? If you felt okay, then maybe try the next dose. If you felt too drowsy? Don’t take the next one. Call your doctor. Your log will show you exactly what happened.
2. Watch for Dangerous Combinations
Alcohol, sleeping pills, muscle relaxers, anti-anxiety meds - all of these slow down your breathing. Opioids do too. Together? That’s how people stop breathing in their sleep.Your log must track every substance, even if it’s “just a glass of wine” or “a Valium my friend gave me.” Write it down. Then look back. If you notice you’ve taken alcohol with opioids more than twice in a week, that’s a red flag. That’s a pattern you need to break.
3. Check Before You Take It
Before you reach for any pill - even a Tylenol - look at your log. Did you take this same drug in the last 4 hours? Did you already take something that makes it stronger? Your log is your second brain. Use it.4. Share It With Someone You Trust
The National Harm Reduction Coalition says one of the best ways to prevent overdose is to never use alone. But what if you’re not using recreationally? What if you’re just taking your prescribed meds?Still, share your log. Give a copy to a family member, friend, or caregiver. Tell them: “If I ever seem too sleepy, or can’t wake up, check this. It’ll tell you what I took.”
This isn’t about control. It’s about safety. If you pass out, they’ll know what to tell paramedics. They might even have naloxone - the overdose-reversal drug - and know when to use it.
Common Mistakes and How to Avoid Them
Most people start a log with good intentions. Then they stop. Here’s why - and how to fix it.Mistake 1: “I’ll remember.”
You won’t. Stress, fatigue, pain, and medications themselves can mess with your memory. Don’t trust yourself. Write it down - even if you think it’s obvious.Mistake 2: “I don’t take enough to overdose.”
Fentanyl - a synthetic opioid 50 to 100 times stronger than morphine - is now found in counterfeit pills that look like oxycodone or Xanax. Even one pill can kill. Your log helps you track what you’re actually taking, not what you think you’re taking.Mistake 3: “I only use it when I’m in pain.”
That’s fine - but pain changes. Some days you need 5mg. Other days, 10mg. Your log shows you what’s working. It also shows you if you’re slowly increasing without realizing it.Mistake 4: “I don’t want to look like I’m addicted.”
Tracking your meds isn’t a sign of addiction. It’s a sign of responsibility. Doctors use logs every day. Pharmacists rely on them. You should too.When to Talk to Your Doctor
Your log isn’t just for you. It’s a tool to help your doctor help you.Bring it to every appointment. Show them:
- How often you’re taking each drug
- When you felt side effects
- Any substances you took with it
- Whether you skipped doses or took extra
This gives them real data - not your best guess. They might adjust your dose, switch you to a safer drug, or recommend a pain management program. If you’re using opioids long-term, your doctor should check your state’s Prescription Drug Monitoring Program (PDMP). But that system only sees what’s prescribed. Your log shows what you actually took.
Real-Life Example: Sarah’s Story
Sarah, 58, from Manchester, was prescribed oxycodone after knee surgery. She also took melatonin for sleep and a muscle relaxant for stiffness. One night, she felt too tired to get up. Her husband found her asleep, barely breathing.Paramedics gave her naloxone. She woke up. Later, they looked at her log - written in a small notebook she kept on her nightstand. It showed she’d taken oxycodone at 8pm, muscle relaxant at 9pm, and melatonin at 10pm. She didn’t realize melatonin could slow breathing too. She thought it was “just a natural sleep aid.”
Her doctor changed her meds. She stopped the muscle relaxant. She switched to a non-sedating sleep option. She kept her log. Six months later, she’s pain-free, sleeping well, and never felt safer.
Your Next Steps
1. Get a notebook - or open a notes app on your phone. 2. Write your first entry - even if you’re not starting a new med. Log what you took today. 3. Set a reminder - 30 minutes after you take your meds, pause and write it down. 4. Share it - give a copy to one person you trust. 5. Bring it to your next doctor’s visit - and ask: “Is this safe with what I’m taking?”You don’t need to be perfect. You just need to be consistent. One entry a day. That’s all it takes.
Overdose doesn’t happen in a moment. It happens because of a chain of small, unnoticed choices. Your medication log breaks that chain. It gives you control. It gives you clarity. And in a world where pills can be deadly even when they’re legal - that’s not just smart. It’s lifesaving.



Matthew Peters
November 19, 2025 AT 16:16I used to think logs were for nerds or people with OCD. Then I started taking gabapentin and tramadol together and nearly passed out watching Netflix. One night I woke up sweating, confused, and realized I had no idea what I’d taken in the last 12 hours. Started writing it down in a shitty notebook I stole from my job. Now I don’t even think about taking a pill without checking it. It’s not about trust-it’s about not dying alone on your couch. 🤡
Liam Strachan
November 19, 2025 AT 23:48Really appreciate this. I’ve got my mum on five different meds and she swears she remembers everything. She doesn’t. I printed out a simple template and stuck it to the fridge. She hates it at first, but now she’ll even ask me to write it for her if she’s feeling foggy. Small thing, big difference. Keep it simple, keep it visible.
Gerald Cheruiyot
November 20, 2025 AT 05:56Medication logs are just the modern version of keeping a journal of your body’s conversation with chemicals. We don’t track calories, sleep, or mood with the same rigor we track our meds-but we should. The body doesn’t lie. It just gets louder when ignored. Your log is the transcript. Read it. Listen. Adjust. Not because you’re sick. Because you’re alive.
Michael Fessler
November 20, 2025 AT 11:21For anyone using polypharmacy-especially with CNS depressants-this is non-negotiable. You need to log not just the Rx but also OTCs, supplements, and even herbal teas. Kava, valerian, and even high-dose magnesium can potentiate opioids and benzos. I’ve seen ER cases where the patient said they ‘only took one’-but the log showed three different sedating agents taken over 8 hours. CYP450 interactions are silent killers. Document everything. Even the ‘harmless’ stuff.
daniel lopez
November 20, 2025 AT 12:38They want you to log your meds because Big Pharma doesn’t want you to know how many of these drugs are just slow poison. The FDA approves them but never tests real-world combos. Your log isn’t for safety-it’s for accountability. Who’s really responsible when you OD on a ‘prescribed’ pill? The doctor? The pharmacist? Or the system that sells you a bottle of death with a smile? Write it down. Then burn the system.
Nosipho Mbambo
November 22, 2025 AT 05:56Ugh. This is so much effort. I mean, I just take my pills. Why do I need to write down ‘10:15-oxycodone 5mg-swallowed-for back pain-no alcohol-felt sleepy’? I’m not a robot. I have a life. Also, I use the same app that reminds me to take them. Isn’t that enough? Why does everything have to be a spreadsheet now? 😩
Katie Magnus
November 22, 2025 AT 09:44Wow. A ‘medication log.’ How quaint. I mean, I’ve been taking opioids for chronic pain for 8 years and I’ve never once written anything down. I just know my body. I know when I need it. I know when I don’t. This feels like someone who’s never had real pain trying to turn survival into a productivity hack. Like, congrats-you turned a medical necessity into a bullet-point checklist. How very Silicon Valley.
Destiny Annamaria
November 23, 2025 AT 10:55My grandma kept a little red book. Every pill. Every time. Even when she was confused, she’d point to it. One night she fell. The paramedics saw the book. They knew she hadn’t taken her blood pressure med that morning. They knew she’d taken her pain med 2 hours early. They stabilized her before the hospital even got her chart. That book saved her life. I started mine last week. It’s not about being perfect. It’s about being prepared. For yourself. For them.