Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t accidents-they’re preventable. Whether you’re taking one pill a day or managing five different prescriptions, how you use your meds matters more than you think. The truth is, medication safety isn’t just up to your doctor or pharmacist. It’s your job too.
Know Exactly What You’re Taking
You wouldn’t drive a car without knowing how the brakes work. Yet most people take pills without understanding what’s inside them. The FDA says you should ask eight key questions every time you get a new prescription: What’s the name? What’s the active ingredient? Why am I taking it? How much and when? What does it look like? When does it expire? What side effects should I watch for? And what should I avoid while taking it-food, alcohol, other drugs?Don’t assume the label tells you everything. Some pills look identical but have wildly different effects. Glimepiride and glyburide, for example, are both diabetes drugs-but mix them up, and your blood sugar could crash. Pharmacists use something called Tall Man Lettering to reduce these errors: predniSONE vs. predniSOLONE. You can do the same. When you pick up a refill, check the name on the bottle against the last one. If it looks different, ask.
Keep a Real-Time Medication List
A 2023 CDC report found that half of all medication errors happen during care transitions-when you move from hospital to home, or see a new doctor. Why? Because no one has the full picture. Your GP doesn’t know about the herbal supplement you take for sleep. The ER nurse doesn’t know you stopped your blood pressure pill last week because you felt fine.Start a simple list. Use your phone or a notebook. Include:
- Drug name (brand and generic)
- Dose (e.g., 10 mg)
- Frequency (e.g., once daily at bedtime)
- Reason (e.g., “for high cholesterol”)
- When you started
- Any over-the-counter meds, vitamins, or supplements
Update it every time you see a provider-even if you think it’s minor. Bring it with you to every appointment. Studies show patients who do this have 40% fewer medication errors.
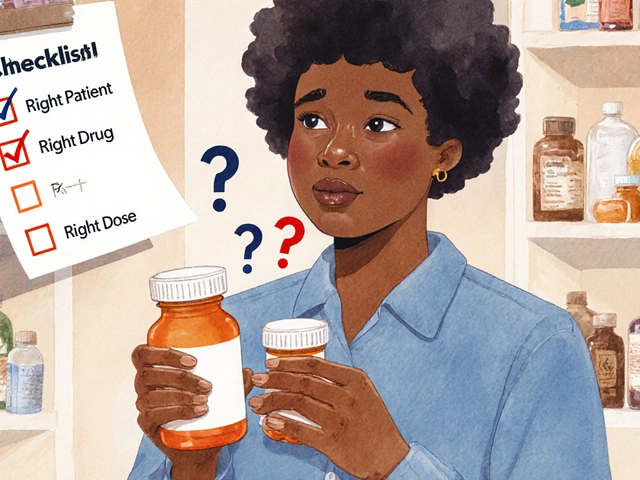
Follow the 5 Rights of Medication Safety
This isn’t just for nurses. It’s for you too. Before you take any pill, ask:- Right patient? Is this medicine really for me? (Don’t grab a pill from your spouse’s bottle.)
- Right drug? Does it match your list?
- Right dose? Is this the amount your doctor ordered?
- Right route? Is it supposed to be swallowed, injected, or applied to the skin?
- Right time? Are you taking it with food? At night? Every 8 hours?
It sounds basic-but when you’re tired, stressed, or juggling multiple meds, these checks make all the difference. One study found that using this checklist reduced errors by 35% in older adults.
Watch Out for High-Risk Medications
Some drugs are more dangerous if used wrong. The Institute for Safe Medication Practices calls these “high-alert medications.” They include:- Insulin
- Warfarin (blood thinner)
- Heparin (injectable blood thinner)
- Intravenous oxytocin (used in labor)
These aren’t just “strong” drugs-they’re error-prone. A wrong dose of insulin can send you into a coma. Too much warfarin can cause internal bleeding. If you take one of these, extra caution is non-negotiable.
Ask your pharmacist: “Is this a high-alert drug?” They’ll know. Use pill organizers with alarms. Set phone reminders. Never refill without checking with your provider. And if you feel off-dizzy, confused, bleeding unusually-call your doctor immediately. Don’t wait.
Never Skip or Stop Without Talking First
You feel better. So you stop taking your antibiotic after three days. Or you skip your blood pressure pill because you don’t like the side effects. Bad idea.The FDA says 23% of antibiotic treatment failures happen because people quit too early. That’s how superbugs form. Stopping blood pressure or heart meds suddenly can trigger a heart attack or stroke. Even antidepressants need to be tapered off slowly.
If a side effect is bothering you-nausea, drowsiness, rash-don’t guess. Call your doctor. There’s often a better option. Maybe a lower dose. Maybe a different drug. But never make the call on your own.
Use Tools That Help, Not Hurt
Technology can be your ally. Pill organizers with compartments for morning, afternoon, and night cut down on missed or double doses. Smartphone apps like the CDC’s free Medication Safety Checklist (launched in January 2024) let you log doses, set reminders, and track side effects.But don’t rely on memory. One Reddit user shared how they confused two diabetes pills for three days-until their blood sugar dropped so low they passed out. A simple pill box with labels could’ve prevented it.
Older adults should do a “medicine cabinet clean-out” twice a year. Expired meds are a hidden danger. The Illinois Department of Public Health found that 38% of accidental poisonings in kids come from old pills left in bathrooms.
Ask for the Teach-Back Method
Too often, patients leave the office with a prescription and no real understanding. Your doctor might say, “Take this twice a day.” But what does that mean? With food? Before bed? What if you miss a dose?Ask them to use the “teach-back” method: “Can you tell me in your own words how to take this?” If you can explain it clearly, you’ve understood. If not, they’ll re-explain. A 2021 study in JAMA Network Open found that patients who went through teach-back had 40% better adherence.
This isn’t about being tested. It’s about making sure you’re safe.

Pharmacists Are Your Hidden Safety Net
Most people think pharmacists just hand out pills. But they’re trained to catch errors your doctor might miss. They know about drug interactions, outdated dosing, and dangerous combinations.When you get a new prescription, ask: “Is this safe with everything else I’m taking?” Don’t assume your doctor knows about your fish oil, turmeric, or CBD. Pharmacists see the full picture. Patients who talk to their pharmacist before starting a new drug have 27% fewer mistakes.
Use them. Ask questions. No question is too small.
What If You Make a Mistake?
You took two pills by accident. You missed a dose. You took the wrong one. Don’t panic. Don’t hide it.Call your pharmacist or doctor. They’ve seen it before. For some drugs, a double dose might be harmless. For others, it’s an emergency. They’ll tell you what to do. Hiding it only makes things worse.
And if you notice someone else-like an elderly parent-struggling with their meds, help them set up a system. It’s not nagging. It’s saving a life.
Final Thought: Safety Is a Habit, Not a One-Time Task
Medication safety isn’t about being perfect. It’s about building habits. Keeping a list. Checking labels. Asking questions. Using reminders. Talking to your pharmacist.People who take five or more medications are over three times more likely to make an error. That’s not because they’re careless. It’s because the system is complex. But you don’t have to be another statistic. Start small. Pick one habit this week-maybe writing down your meds or setting a phone alarm. Do it every day. Then add another.
Every pill you take correctly is one less trip to the ER. One less scare. One more day of feeling well.
What should I do if I miss a dose of my medication?
Don’t double up unless your doctor says to. Check the medication guide or call your pharmacist. For some drugs, like antibiotics, missing a dose can reduce effectiveness. For others, like blood pressure meds, it’s usually safe to take it as soon as you remember, unless it’s almost time for the next dose. Never guess-ask.
Can I crush or split my pills?
Only if the label or your pharmacist says it’s okay. Some pills are designed to release medicine slowly. Crushing them can cause too much drug to enter your system at once. Others have coatings to protect your stomach. Always check before altering a pill.
Why do I need to know my medication’s active ingredient?
Many drugs have the same active ingredient under different brand names. Taking two with the same active ingredient-like acetaminophen-can lead to overdose. Knowing the ingredient helps you avoid duplicates and spot dangerous combinations.
How often should I update my medication list?
Update it every time you see a healthcare provider-even for a cold or a checkup. Also update it after any pharmacy refill, if you start or stop a supplement, or if your dose changes. Keep it in your phone and wallet so it’s always handy.
Are over-the-counter drugs and supplements safe to take with prescriptions?
Not always. Common supplements like St. John’s Wort, garlic, and ginkgo can interfere with blood thinners, antidepressants, and blood pressure meds. Even vitamin K can make warfarin less effective. Always tell your doctor and pharmacist everything you take-even if you think it’s “natural” or “harmless.”
What’s the best way to dispose of old or expired medications?
Don’t flush them or throw them in the trash. Use a drug take-back program-many pharmacies and police stations offer them. If none are available, mix pills with coffee grounds or cat litter in a sealed bag before tossing. This makes them unappealing and unsafe for kids or pets to find.
Why do I need to check the appearance of my pills each time I refill?
Pills can look different between manufacturers-even if they’re the same drug. A change in color, shape, or markings doesn’t always mean it’s wrong-but it’s a red flag to check. One person took a different version of their cholesterol pill and didn’t realize it until they felt dizzy. Always compare your new pills to the last refill.
Can I share my prescription meds with someone else?
Never. A drug that helps you could harm someone else. Doses are based on weight, age, health conditions, and other meds. Sharing prescriptions is illegal and dangerous. Even if you think it’s a “little” pill, it could cause a serious reaction.
What should I do if I think I’m having a bad reaction to a drug?
Call your doctor or pharmacist right away. If you have trouble breathing, swelling of the face or throat, chest pain, or sudden confusion, go to the ER or call emergency services. Don’t wait to see if it gets better. Some reactions can turn deadly in minutes.
How long does it take to get good at managing medications?
Most people need 3 to 5 visits with their care team to build reliable habits. For older adults or those on complex regimens, it can take 7 or more follow-ups. It’s not about being smart-it’s about practice. Use tools, ask questions, and keep going. Safety builds over time.
Medication safety isn’t about fear. It’s about control. You’re not just taking pills-you’re managing your health. And with the right habits, you can do it without risk.

Shante Ajadeen
November 13, 2025 AT 23:20Just started using a pill organizer with alarms after my grandma almost mixed up her blood pressure meds. Best decision ever. Now I set reminders for everything-even my daily vitamin. Feels like a small thing, but it’s saved me from panic more than once.
edgar popa
November 15, 2025 AT 04:48took my meds wrong once. almost died. now i double check. no cap.
Alex Ramos
November 16, 2025 AT 07:06My pharmacist caught that I was doubling up on acetaminophen because I didn’t know the cold med had it too. She didn’t judge, just handed me a free printable med tracker. That’s why I always ask ‘is this safe with everything else?’ even if I feel dumb asking. They’ve seen it all.
Erica Cruz
November 16, 2025 AT 12:24Let’s be real-this whole ‘medication safety’ thing is just corporate propaganda to sell you apps and pill organizers. The real problem? Doctors overprescribing and pharma hiding side effects. You think a checklist fixes systemic greed? LOL. I’ve been on 7 meds for 12 years. I don’t need a pamphlet to know most of them are unnecessary.
Johnson Abraham
November 17, 2025 AT 01:47lol so now we gotta write down every pill like its a college class? smh. i just take em when i remember. if i feel weird? i stop. problem solved. 🤷♂️
Mark Rutkowski
November 18, 2025 AT 11:05Medication isn’t just chemistry-it’s rhythm. It’s the quiet dance between your body and the molecules they put inside you. Every pill is a promise. A promise to be seen, to be cared for, to be understood. When we treat meds like groceries, we forget we’re not just managing symptoms-we’re honoring our own survival. Maybe that’s why the ‘5 Rights’ feel so sacred. It’s not about rules. It’s about reverence.
Ryan Everhart
November 20, 2025 AT 09:10So you're telling me the same person who forgets to pay their phone bill is supposed to remember 12 different pills with 3 different schedules? And if they mess up? It's their fault? Cool. Meanwhile the system charges $200 for a 10-minute consult to explain what the label already says in 8-point font. Yeah. I'm sure it's just about habits. 😏
Deepa Lakshminarasimhan
November 21, 2025 AT 19:10Did you know the FDA doesn’t require drug manufacturers to test how their pills interact with every single supplement on the market? And most pharmacies don’t even have the software to flag all the hidden combos? I read a whistleblower report last year-half the time, the ‘drug interaction alerts’ are turned off because they’re too noisy. So yeah, keep your list. But don’t trust the system. Trust yourself. And maybe keep a notebook hidden under your mattress. Just in case.
dace yates
November 21, 2025 AT 22:29I’m curious-how do you define ‘high-alert’ meds? Is it based on FDA classification or actual error rates? I’ve seen insulin flagged everywhere, but what about lithium or digoxin? Are those equally dangerous? I ask because my aunt takes both and no one ever mentions them.
Danae Miley
November 22, 2025 AT 15:49There is a critical omission here: the lack of standardized electronic health record interoperability across pharmacies and providers. Without real-time, bidirectional data sharing, patient-generated lists are inherently unreliable. You cannot mitigate systemic fragmentation with behavioral checklists alone. The burden is misplaced. This is a policy failure, not a personal one.
David Barry
November 23, 2025 AT 22:36My cousin took his wife’s blood thinner because he thought it was ‘just a vitamin.’ He bled internally for three days before he told anyone. They had to pump his stomach. He’s fine now. But you know what? He didn’t even know it was warfarin. The bottle said ‘blood pressure pill.’ That’s the problem. Labels lie. People lie. Systems lie. You think your checklist fixes that? It doesn’t. It just makes you feel better while the machine keeps grinding.
Eve Miller
November 25, 2025 AT 22:20It’s disgusting how many people treat their prescriptions like candy. I’ve seen people post online about ‘sharing’ ADHD meds with friends. That’s not just irresponsible-it’s criminal. And you wonder why ERs are packed? It’s because people think their body is a video game and they can respawn after a bad dose. Wake up. This isn’t a suggestion. It’s life or death.
Chrisna Bronkhorst
November 26, 2025 AT 04:28My dad took his heart med twice by accident. He didn’t say anything for 12 hours. Said he didn’t want to bother anyone. He ended up in ICU. Now I check his meds every morning. No drama. No yelling. Just ‘Dad, did you take it?’ And he says yes. And I know he’s safe. It’s not about control. It’s about love.
Alyssa Lopez
November 26, 2025 AT 22:33Y’all need to stop being so soft. In America we don’t coddle people with pill boxes and teach-backs. We teach them to be responsible. If you can’t manage your meds? Maybe you shouldn’t be on them. This country is drowning in weak-minded compliance culture. Take the pill. Don’t cry. Move on. Stop making everything a support group.