Hodgkin's Disease Stage Explorer
Stage I
Single lymph node region
Stage II
Two or more adjacent regions
Stage III
Involvement above and below diaphragm
Stage IV
Disseminated disease
Stage Information
Select a stage above to view detailed information.
Understanding B Symptoms
B symptoms indicate more aggressive disease behavior:
- Fever >38°C (100.4°F) for more than 24 hours
- Night Sweats that soak clothing
- Weight Loss >10% body weight over six months
Presence of B symptoms affects staging (e.g., I B, II B) and often leads to more intensive treatment.
Quick Takeaways
- Hodgkin's disease is staged from I to IV using the AnnArbor system.
- Early stages (I‑II) often need only radiation or a short chemotherapy course.
- Advanced stages (III‑IV) require combined chemo‑radiation and close monitoring.
- B symptoms-fever, night sweats, weight loss-affect staging and treatment decisions.
- Overall 5‑year survival exceeds 85% when treated promptly.
When doctors talk about Hodgkin's disease is a type of lymphoma that starts in the lymphatic system, often marked by the presence of Reed‑Sternberg cells. Understanding how it progresses through the Hodgkin's disease stages helps patients, families, and caregivers make sense of diagnosis, treatment options, and long‑term outlook.
What Is Hodgkin's Disease?
Also called Hodgkin lymphoma, this cancer originates in lymph nodes and can spread to nearby organs. The hallmark is the Reed‑Sternberg cell a large, abnormal B‑cell with a distinctive ‘owl‑eye’ nucleus that pathologists look for under the microscope. While it accounts for only about 0.5% of all cancers, it’s one of the most curable adult cancers when caught early.
How Doctors Stage Hodgkin's Disease
Staging follows the AnnArbor system, which grades disease based on the number and location of lymph node groups involved and whether the cancer has spread beyond the lymphatic system. Imaging-primarily a PET‑CT scan a combined positron emission tomography and computed tomography that highlights metabolically active tissue.-is the gold standard for accurate staging.
Stage I: Single Lymph Node Region
In StageI, cancer is limited to one lymph node group (e.g., cervical, mediastinal) or a single organ outside the nodes. Patients often feel a painless lump and may have no systemic symptoms.
Treatment usually involves involved‑field radiation or a brief course of ABVD chemotherapy a regimen of doxorubicin, bleomycin, vinblastine, and dacarbazine. The 5‑year survival for StageI exceeds 95%.
Stage II: Two or More Adjacent Regions
StageII spreads to two or more lymph node groups on the same side of the diaphragm (above or below). B symptoms, if present, upgrade the stage to “IIE” or “IIA”.
Most clinicians combine radiation therapy high‑energy beams that target tumor‑bearing areas while sparing surrounding tissue. with 2-4 cycles of ABVD. Survival remains around 90%.

Stage III: Involvement Above and Below the Diaphragm
StageIII means cancer spans lymph node groups on both sides of the diaphragm, often affecting the spleen or mediastinum.
Standard care is 4-6 cycles of ABVD followed by involved‑site radiation for bulky disease. The 5‑year survival drops to about 80%, but many patients are cured.
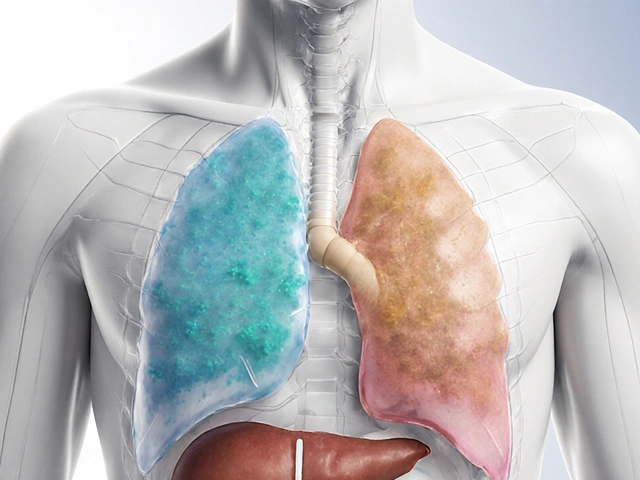
Stage IV: Disseminated Disease
StageIV indicates that Hodgkin's disease has spread to distant organs such as the liver, bone, or lungs. Symptoms can be more severe, including persistent cough, shortness of breath, or organ‑specific pain.
Intensive chemotherapy-often escalated BEACOPP (bleomycin, etoposide, Adriamycin, cyclophosphamide, vincristine, procarbazine, prednisone)-is the mainstay, sometimes followed by high‑dose therapy and stem‑cell rescue. Survival rates hover around 70% but continue to improve with newer agents.
B Symptoms and Their Impact on Staging
‘B symptoms’ are systemic signs that influence stage categorization:
- Unexplained fever >38°C (100.4°F) for more than 24hours
- Drastic night sweats that soak clothing
- Weight loss of >10% body weight over six months
If any of these appear, the stage gains a “B” suffix (e.g., IB, IIB). Presence of B symptoms often nudges clinicians toward adding chemotherapy, even in early stages, because they suggest a more aggressive disease biology.
Treatment Options by Stage
Below is a quick comparison of typical regimens:
| Stage | Typical Therapy | Key Drugs / Modality | 5‑Year Survival |
|---|---|---|---|
| I | Radiation alone or 2 cycles ABVD | Radiation, ABVD | ~95% |
| II | Combined chemo‑radiation | ABVD + involved‑site radiation | ~90% |
| III | ABVD (4-6 cycles) ± radiation | ABVD, Radiation (bulky disease) | ~80% |
| IV | Escalated BEACOPP or ABVD + possible stem‑cell transplant | BEACOPP, ABVD, Autologous transplant | ~70% |
Prognosis and Long‑Term Outlook
Overall, Hodgkin's disease boasts one of the highest cure rates among adult cancers. Factors that improve prognosis include:
- Early stage at diagnosis (I‑II)
- Absence of B symptoms
- Limited bulk disease
- Younger age (under 45) and good performance status
Late relapses can occur 10-15years after treatment, so survivorship programs focus on regular imaging, blood work, and monitoring for secondary malignancies caused by prior radiation.
Follow‑Up Care and Monitoring
After completing therapy, most patients undergo a PET‑CT at 6‑12weeks to confirm remission. Subsequent scans are typically scheduled every 6‑12months for the first two years, then annually up to five years.
Blood tests track organ function-especially liver enzymes and thyroid levels-since some chemotherapy agents can affect those systems. Lifestyle advice (balanced diet, smoking cessation, limited alcohol) helps reduce the risk of secondary cancers.

Frequently Asked Questions
What are the early signs of Hodgkin's disease?
Most people first notice a painless lump in the neck, armpit, or groin. Some also report fatigue or mild night sweats before the disease spreads.
How is staging performed?
Staging relies on physical examination, blood work, and imaging-especially PET‑CT scans. A biopsy confirms the presence of Reed‑Sternberg cells, and the AnnArbor system classifies the spread.
What does StageII mean for treatment?
StageII involves two or more adjacent lymph node groups on the same side of the diaphragm. Treatment usually combines ABVD chemotherapy with localized radiation, giving a cure rate above 90%.
Can Hodgkin's disease be cured?
Yes-especially when caught at StageI orII. Even in advanced stages, modern chemo‑radiation protocols achieve long‑term remission in a majority of patients.
What are B symptoms and why do they matter?
B symptoms are fever, night sweats, and weight loss. Their presence upgrades a stage (e.g., IB) and often leads clinicians to add chemotherapy because they signal a more aggressive disease.
How often are scans needed after treatment?
A PET‑CT is done 6‑12weeks post‑therapy. If the scan is clear, follow‑up imaging occurs every 6‑12months for the first two years, then annually up to five years, unless symptoms reappear.

Akhil Khanna
October 3, 2025 AT 18:29Hey all, great rundown on the stages – super helpful for anyone just hearing about Hodgkin’s for the first time 😊. Remember to ask your docc about PET‑CT scans, they’re key for accurate staging.
Zac James
October 7, 2025 AT 18:29The article does a solid job bridging medical detail with lay‑person clarity, which is valuable across cultures.
Arthur Verdier
October 11, 2025 AT 18:29Oh sure, because the world really needed another exhaustive guide on Hodgkin’s staging.
Apparently the secret to curing cancer lies in memorizing whether the disease is I, II, III, or IV.
What about the hidden agenda behind those fancy PET‑CT machines?
They say the scanners are for accurate staging, but who’s to say they aren’t tracking our movements for a grand surveillance plan?
And those B‑symptoms? Just a clever marketing ploy to sell more antihistamines.
You think the “Reed‑Sternberg” cell is a scientific term, not a code word for something far more sinister.
The survival rates sound optimistic, yet they conveniently ignore the long‑term side effects that pharmaceutical companies love to hide.
Don’t be fooled by the “95 % five‑year survival” – it’s a number cooked up by PR departments.
Ever notice how every breakthrough comes with a new cocktail of chemo drugs whose names sound like a bad sci‑fi series?
BEACOPP, ABVD, who even knows what they stand for, but they’re definitely made to keep the pharmaceutical profits soaring.
Radiation therapy? Just another way to turn patients into walking radios.
And the follow‑up scans-another subscription service for hospitals.
So, when the article says early detection is key, remember that key might unlock a different kind of door.
Stay skeptical, question the protocols, and maybe keep your own health data off the cloud.
In the end, the only thing we’re really guaranteed is that someone will always have a reason to write another article like this.
Breanna Mitchell
October 15, 2025 AT 18:29This info really lifts my spirits-thanks for sharing!
joni darmawan
October 19, 2025 AT 18:29The presentation balances clinical precision with accessible language, which is commendable. Moreover, the philosophical underpinnings of staging reflect an attempt to categorize complexity within a manageable framework. Such clarity aids both practitioners and patients in navigating treatment pathways.
Richard Gerhart
October 23, 2025 AT 18:29If you’re looking for practical tips, start by asking your oncologist about the specific chemo regimen-ABVD or BEACOPP-depending on the stage. Also, keep an eye on your blood work; those chemo drugs can be rough on the liver. Don’t forget to schedule regular follow‑up PET scans, they’re essential. And yeah, some of the medical jargon can feel like a foreign language, but you’ll pick it up quick.
Kim M
October 27, 2025 AT 17:29💀 Ever wonder why the pharma lobby pushes BEACOPP like it’s the only answer? The truth is probably deeper than the brochure. 🌐
Martin Gilmore
October 31, 2025 AT 17:29I must point out-excessive punctuation!!!, and the over‑use of jargon, can obscure meaning; it’s a travesty!!! The article could have been concise, but instead it drags on-ridiculous!!!
jana caylor
November 4, 2025 AT 17:29The data presented is thorough and well‑structured. It provides a solid foundation for further discussion.
Vijendra Malhotra
November 8, 2025 AT 17:29This post is solid, but the tone could be more aggressive in calling out outdated protocols. Also, grammar is spotless, kudos!
Amy Aims
November 12, 2025 AT 17:29Love how the guide mixes science with empathy 😊. Keep the balanced tone, it really helps patients feel hopeful!
Shaik Basha
November 16, 2025 AT 17:29Yo, good job breaking down the stages, but watch those misspeals-like “chemo” vs “chemootherapy”. Also, keep it real, man.
Michael Ieradi
November 20, 2025 AT 17:29Respectfully, the article offers a comprehensive overview; however, I would suggest a brief summary at the beginning - it would aid quick reference.
Stephanie Zuidervliet
November 24, 2025 AT 17:29Honestly, the whole thing feels like a dramatized lecture-so much hype for a routine medical explanation!!!
Olivia Crowe
November 28, 2025 AT 17:29Your optimism shines through, making a tough subject feel manageable.
Aayush Shastri
December 2, 2025 AT 17:29Great effort in making the information accessible across cultures; let’s continue sharing such resources. And remember, community support makes the journey easier.