Amiodarone-Digoxin-Warfarin Dose Adjuster
When starting amiodarone in patients already taking digoxin and warfarin, precise dose adjustments are critical to prevent life-threatening toxicity. This tool calculates the recommended dose reductions based on current medications.
Recommended Adjustments
Enter your current doses to see recommended adjustments.
Critical Monitoring Guidelines
• Check digoxin levels 72 hours after starting amiodarone
• Test INR every 48-72 hours for first two weeks
• In elderly patients, keep digoxin levels < 1.0 ng/mL
• Monitor for nausea, blurry vision, or irregular heartbeat
When a patient is on amiodarone, digoxin, and warfarin at the same time, something dangerous is happening beneath the surface - even if they feel fine. This isn’t just a textbook warning. It’s a real, life-threatening combo that shows up in hospitals every week. And it’s often missed because the symptoms sneak up slowly. A 78-year-old man on warfarin for atrial fibrillation starts feeling nauseous after a new amiodarone script. His doctor checks his INR - it’s 9.4. He’s bleeding internally. His digoxin level? 3.1 ng/mL. Toxic. He almost didn’t make it. This isn’t rare. It’s predictable. And it’s preventable.
Why This Triad Is So Deadly
Amiodarone doesn’t just sit there. It changes how your body handles other drugs. It’s like a silent saboteur in your liver and kidneys. When you take amiodarone with digoxin, digoxin levels can jump by 70% in just a few days. That’s not a small bump. That’s the difference between a safe dose and a lethal one. Digoxin toxicity doesn’t just cause dizziness. It causes vomiting, blurry yellow vision, and chaotic heart rhythms that can kill you. And when amiodarone teams up with warfarin? Your blood stops clotting - hard. INR levels that were stable at 2.5 can rocket to 8 or higher without any dose change. One study found 28% higher death rates in patients on this combo compared to those on digoxin alone. That’s not a coincidence. That’s pharmacology in overdrive.How Amiodarone Breaks Your Body’s Balance
Amiodarone is built to last. Its half-life? Up to 100 days. That means once it’s in you, it’s not leaving anytime soon. And it doesn’t just stick around - it interferes. It blocks P-glycoprotein, a transporter that normally pushes digoxin out of your cells. Without that push, digoxin piles up in your blood. It also shuts down CYP2C9, the main enzyme that breaks down warfarin. S-warfarin, the more powerful half of the drug, gets cleared 55% slower. That’s why your INR spikes. Even worse, high digoxin levels can knock warfarin off its protein bindings, freeing up even more active drug. It’s a triple hit: more digoxin, more warfarin, and less way out. No wonder bleeding and arrhythmias happen together.What Happens When You Don’t Adjust Doses
Here’s what goes wrong in real life. A patient on 0.125 mg of digoxin daily for AFib. Stable. Then they start amiodarone. No one tells them to cut the digoxin. Three days later, they’re vomiting. Four days later, their ECG shows bidirectional ventricular tachycardia - a classic digoxin toxicity sign. Meanwhile, their warfarin dose hasn’t changed. Their INR was 2.3 last week. Now it’s 7.8. They fall. A subdural hemorrhage. ICU. This isn’t hypothetical. The FDA’s Adverse Event Reporting System logged over 1,800 digoxin toxicity cases linked to amiodarone between 2010 and 2022. In one study of 12,745 warfarin users, those on amiodarone had a 320% higher chance of INR above 4.0. That’s not a risk. That’s a guarantee of trouble if you don’t act.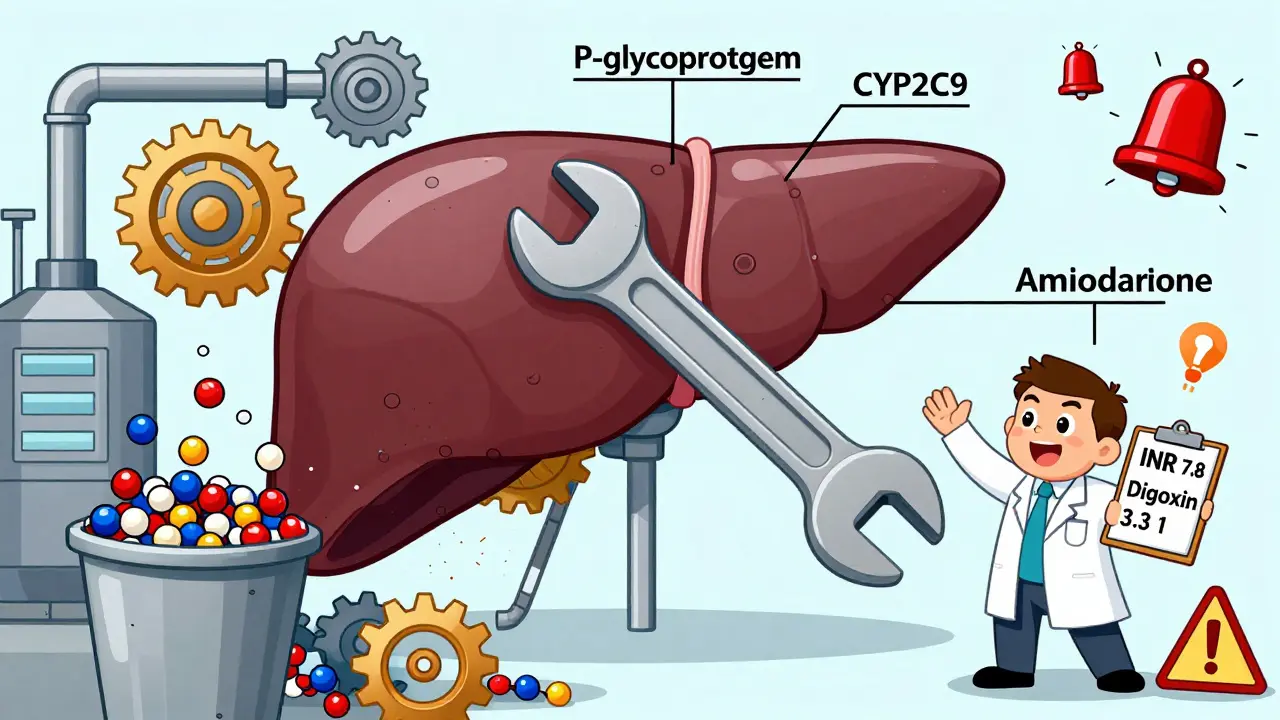
The Exact Steps to Stay Safe
If you’re managing this combo - or if you’re the patient - here’s what you must do. No guesses. No delays.- When starting amiodarone: Cut the digoxin dose in half immediately. Don’t wait for labs. Don’t wait for symptoms. If they were on 0.25 mg, drop to 0.125 mg. If they were on 0.125 mg, drop to 0.0625 mg.
- Check digoxin levels: Get a blood test 72 hours after starting amiodarone. Repeat weekly until stable. In elderly patients, keep levels under 1.0 ng/mL - not 1.2. The margin is razor-thin.
- Reduce warfarin before amiodarone: Drop the warfarin dose by 30-50% before you even give the first amiodarone pill. If they were on 5 mg daily, go to 2.5 mg. If they were on 7.5 mg, go to 3.75 mg.
- Monitor INR like a hawk: Test every 48 to 72 hours for the first two weeks. Then weekly for at least four weeks. Don’t rely on a single number - look at the trend. A jump from 2.8 to 4.2 in 72 hours? That’s a red flag.
- After stopping amiodarone: Keep monitoring. The drug lingers. INR can still rise for 2-4 weeks after the last dose. Keep checking INR for at least 4-6 weeks.
These steps aren’t optional. They’re the minimum. A 2023 NHS England report showed that following this exact protocol cut adverse events by 78% across 47 hospitals. That’s not luck. That’s science.
Why This Still Matters in 2026
You might think: “But everyone uses DOACs now.” True. Dabigatran, apixaban, rivaroxaban - they’ve replaced warfarin in 82% of new AFib cases. But that’s new patients. What about the 4.3 million Americans still on warfarin? Many have mechanical heart valves. Many can’t afford DOACs. Many were started on warfarin years ago and never switched. And amiodarone? It’s still the most effective drug for stubborn arrhythmias. So this triad isn’t fading. It’s growing. Older patients. More polypharmacy. More frailty. More falls. More bleeding. The FDA reported 387 deaths tied to this combo in 2022 - up 12% from the year before. That’s not progress. That’s a system failure.
What You Need to Watch For
Digoxin toxicity isn’t always dramatic. It starts with nausea. Then fatigue. Then blurred vision - especially yellow-green halos around lights. Constipation. Confusion. These are easy to blame on aging. But if someone is on this trio, they’re not just aging. They’re at risk. Watch for irregular heartbeats - especially ventricular tachycardia. That’s a medical emergency. Warfarin over-anticoagulation? Bruising that won’t fade. Nosebleeds that won’t stop. Blood in urine or stool. Headaches that feel worse than ever. A fall with a head bump? That’s not a minor incident. That’s a potential intracranial bleed waiting to happen. INR above 4.0? That’s a code red. You need vitamin K. Maybe fresh frozen plasma. And you need it now.Technology Can Help - But Not Replace
Electronic health records now flag this interaction. That’s good. But flags get ignored. Alerts get bypassed. A 2022 JAMA study found that even with alerts, 40% of high-risk combinations still got prescribed. Why? Because the system didn’t tell the doctor what to do next. It just said, “Warning.” That’s not enough. The fix isn’t more alerts. It’s clear, step-by-step protocols built into the workflow. Cut digoxin. Reduce warfarin. Test INR in 72 hours. That’s the script. And it needs to be automatic - not optional.What to Do If You’re Already on This Combo
If you’re currently taking all three, don’t panic. But don’t wait either. Talk to your doctor. Ask: “Have my digoxin and warfarin doses been adjusted since I started amiodarone?” If they say no - or if they don’t know - push for a full review. Get your digoxin level tested. Get your INR checked. Bring this article with you. This isn’t about fear. It’s about control. You don’t have to live on the edge of a bleeding risk or a toxic heart rhythm. There’s a safer way. And it’s simple: adjust the doses. Monitor closely. Stay ahead.Can I stop warfarin if I’m on amiodarone and digoxin?
No - you shouldn’t stop warfarin without medical supervision. Stopping it suddenly raises your risk of stroke, especially if you have atrial fibrillation. Instead, reduce the dose by 30-50% when starting amiodarone and monitor INR closely. Switching to a DOAC like apixaban may be an option, but only if your doctor confirms it’s safe for your condition (e.g., mechanical heart valves still require warfarin).
How long does it take for amiodarone to affect digoxin and warfarin?
Digoxin levels can rise within 2-7 days. Warfarin’s effect starts showing in INR changes within 3-5 days. But because amiodarone stays in your body for weeks to months, these effects continue long after you start the drug - and even after you stop it. That’s why monitoring must last 4-6 weeks after discontinuing amiodarone.
Is this interaction worse in older adults?
Yes - significantly. Older adults have lower kidney function, less muscle mass, and more fragile blood vessels. Digoxin toxicity is more common at lower levels in the elderly (above 1.0 ng/mL). Warfarin also causes more bleeding in older patients. Over 60% of serious cases involve people over 75. Dose reductions must be more aggressive in this group.
Can I use a different antiarrhythmic instead of amiodarone?
Possibly. Drugs like dronedarone or beta-blockers (e.g., metoprolol) may be alternatives, but they’re not as effective for life-threatening arrhythmias. Amiodarone is often the last resort when others fail. The choice depends on your specific heart rhythm problem. Never switch on your own. Talk to your cardiologist about whether a safer option exists for your case.
What should I do if I miss a dose of amiodarone?
Don’t double up. Take the missed dose if it’s within 12 hours of when you were supposed to take it. If it’s later, skip it and resume your regular schedule. Missing one dose won’t immediately change your digoxin or warfarin levels - but stopping and restarting amiodarone repeatedly can cause dangerous fluctuations. Consistency matters more than perfection.



