Why Timing Matters Between Magnesium and Osteoporosis Pills
If you’re taking a bisphosphonate like Fosamax, Actonel, or Boniva for osteoporosis, and you also take magnesium supplements - whether for muscle cramps, sleep, or general health - you could be quietly sabotaging your treatment. It’s not a myth. It’s not a guess. It’s science. And the stakes are high: magnesium can cut the absorption of your osteoporosis medication by up to 60%, leaving your bones unprotected and your fracture risk unchanged.
This isn’t about being perfect. It’s about being smart. Millions of people take both magnesium and bisphosphonates. Many don’t realize they’re taking them at the same time. And when they do, their bone density doesn’t improve - not because the drugs don’t work, but because they never got absorbed.
How Magnesium Blocks Osteoporosis Drugs
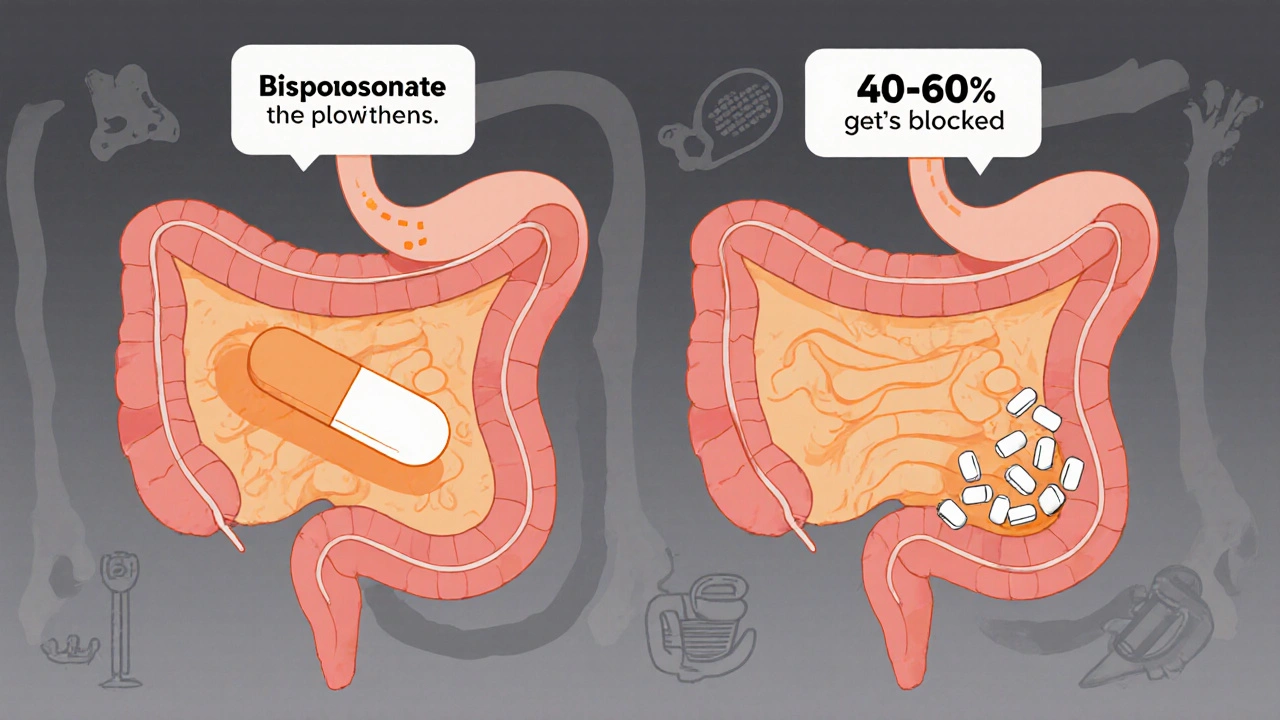
Bisphosphonates are designed to stick to bone and slow down the cells that break it down. But to do that, they have to get into your bloodstream first. And that only happens if they’re absorbed in your stomach and small intestine.
Magnesium, whether from a pill, antacid, or laxative, binds to bisphosphonates in your gut. Think of it like two magnets snapping together. Once they stick, they form a compound your body can’t absorb. That means your Fosamax or Actonel just passes through you - useless.
Studies show that taking magnesium at the same time as a bisphosphonate reduces absorption by 40-60%. That’s not a small drop. That’s the difference between a drug that works and one that doesn’t. The FDA, NIH, and major bone health societies all agree: this interaction is real, measurable, and dangerous if ignored.
What Counts as a Magnesium Source?
You might think only supplements matter. But magnesium is hiding in plain sight.
- Antacids: Milk of Magnesia, Maalox, Mylanta - each contains 400-800mg of magnesium per dose.
- Laxatives: Many over-the-counter constipation treatments are magnesium-based.
- Dietary supplements: Magnesium citrate, glycinate, oxide - any form counts.
- Bottled water: Some brands like San Pellegrino have over 50mg of magnesium per liter.
- Multivitamins: Many include magnesium, even if you don’t realize it.
One patient on Reddit shared how she took Fosamax every Sunday and a magnesium pill every night - thinking she was safe. But she also took Maalox for heartburn every day. That daily antacid was blocking her osteoporosis treatment. Her bone density dropped 8% in a year.
The 2-Hour Rule: What You Need to Do
The standard advice from the NIH, WebMD, and the National Osteoporosis Foundation is clear: separate magnesium and bisphosphonates by at least two hours.
But here’s the catch: bisphosphonates themselves have strict rules. You take them first thing in the morning, on an empty stomach, with a full glass of water. Then you have to wait 30 minutes before eating, drinking, or taking anything else - including coffee, juice, or calcium.
So here’s the real-world timing that works:
- 7:00 AM: Take your bisphosphonate with 8 oz of plain water.
- 7:30 AM: Eat breakfast, drink coffee, take other meds.
- 9:30 AM: Now it’s safe to take your magnesium supplement.
That’s a full two hours after your bisphosphonate - and well after the 30-minute fasting window. This gives your body time to absorb the drug before magnesium enters the system.
If you take your bisphosphonate at night (some formulations allow this), wait two hours after the dose before taking magnesium. Don’t take magnesium right before bed if you’re on a nighttime bisphosphonate - you might fall asleep and forget the gap.
What About IV Osteoporosis Drugs?
If you’re getting zoledronic acid (Reclast) or ibandronate (Boniva) through an IV, you don’t need to worry. These bypass your gut entirely. Magnesium supplements won’t interfere. But if you’re still taking oral bisphosphonates - even just one a month - the rule still applies.
Some people switch to IV treatments because they can’t stick to the timing. That’s fine. But if you’re still on pills, the two-hour rule isn’t optional. It’s essential.
Why People Fail at This - And How to Succeed
A 2022 survey by the National Osteoporosis Foundation found that 37% of people taking both magnesium and bisphosphonates didn’t know they couldn’t take them together. Another 22% admitted they sometimes took them at the same time.
Why? Because it’s hard.
- You’re on five medications. You’re tired.
- You don’t remember which pill is which.
- You think ‘natural’ magnesium from food doesn’t count - but it does.
- Your doctor said ‘avoid calcium’ but never mentioned magnesium.
Here’s what works:
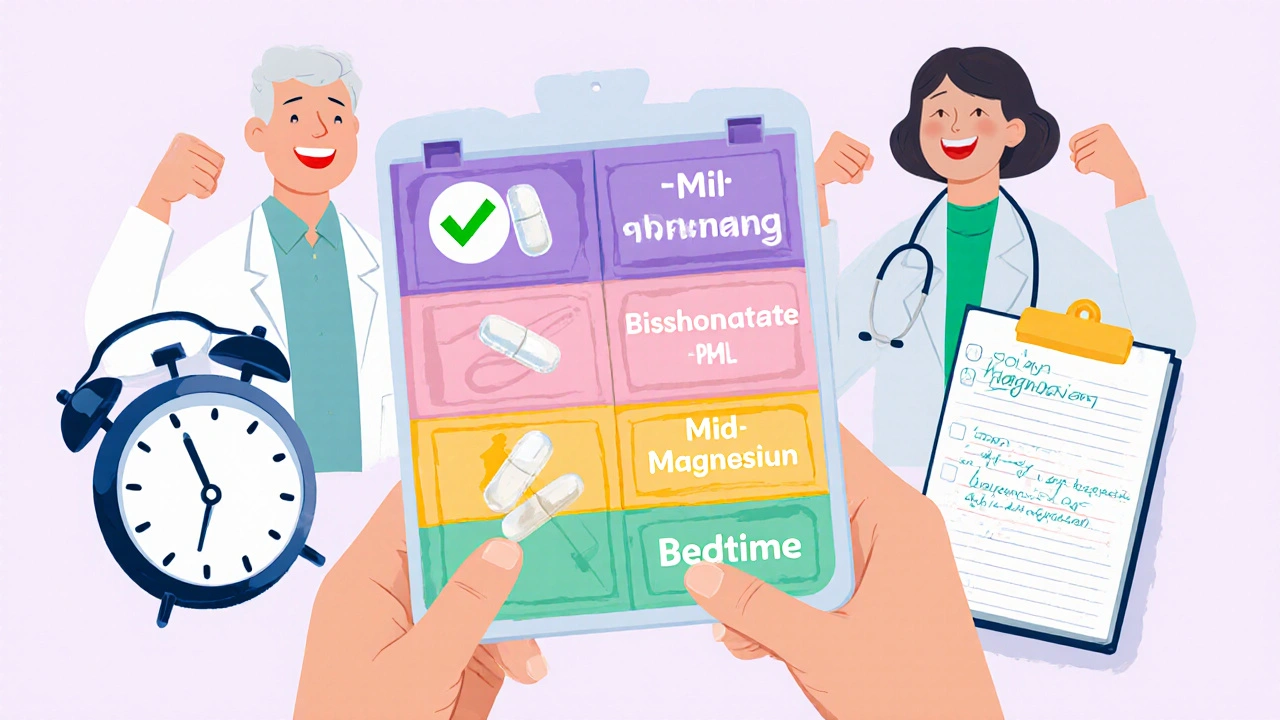
- Use a pill organizer with 4 compartments: AM, mid-morning, PM, bedtime. Put your bisphosphonate in the AM slot, magnesium in mid-morning.
- Set phone alarms: One for your bisphosphonate, another for magnesium two hours later.
- Write it down: Keep a small log next to your meds. Check off each dose.
- Ask your pharmacist: They’re trained to catch these interactions. Don’t assume they know your full list - tell them everything you take.
Hospitals and clinics that use visual ‘timing wheels’ - circular charts showing when to take each drug - see 67% adherence. Those who just get a handout? Only 32% follow the rules.
What Happens If You Don’t Follow the Rule?
It’s not just about ‘less effectiveness.’ It’s about broken bones.
Studies show patients who take magnesium too close to their bisphosphonate have up to 50% less improvement in bone density. Over two years, that means you’re not building protection - you’re just waiting for the next fracture.
Dr. Felicia Cosman, a leading bone specialist, calls this the ‘single largest preventable cause of treatment failure.’ That’s not hyperbole. That’s data. And it’s why the Institute for Safe Medication Practices lists this interaction as a ‘high-alert’ - meaning it’s one of the most dangerous drug mistakes in medicine.
One man in his 70s took Fosamax and magnesium daily for six years. He thought he was doing everything right. His bone density scan showed no improvement. He broke his hip. The doctor found out he’d been taking magnesium with his pill all along.
What’s Changing in the Future?
Drug companies are working on solutions. Merck is testing a new time-release bisphosphonate that’s less affected by minerals. Smart pill bottles with Bluetooth reminders are already helping patients in pilot programs - 92% adherence in one Mayo Clinic study.
By 2025, all U.S. pharmacies will be required to use a standardized counseling script when dispensing bisphosphonates. Pharmacists will be trained to ask: ‘Do you take magnesium? Antacids? Laxatives?’
But you don’t have to wait. Right now, you have the power to protect your bones. You just need to know when to take your pills - and when to wait.
Key Takeaways
- Magnesium blocks bisphosphonates - your osteoporosis medication - by forming an insoluble compound in your gut.
- Always separate magnesium and bisphosphonates by at least two hours.
- Magnesium isn’t just in supplements - it’s in antacids, laxatives, and even some bottled water.
- IV osteoporosis drugs (like Reclast) are not affected - but oral ones are.
- Failure to separate them can lead to zero bone density improvement and higher fracture risk.
- Use alarms, pill organizers, and written logs to stay on track.
Can I take magnesium and Fosamax at the same time if I wait longer than two hours?
Waiting longer than two hours is fine - and even safer. Two hours is the minimum. If you take your Fosamax at 7 AM and your magnesium at 11 AM, you’re well within the safe window. The goal is to make sure your stomach has fully cleared the bisphosphonate before magnesium enters the system. More time = less risk.
Does magnesium from food like spinach or almonds interfere?
No. The interaction only happens with high-dose, supplemental magnesium - typically 200mg or more at once. The amount in food is too low to cause interference. You can eat spinach, almonds, or black beans with your bisphosphonate. Just avoid pills, antacids, or laxatives containing magnesium.
I take calcium supplements too. Do I need to wait for those as well?
Yes. Calcium also blocks bisphosphonate absorption. The same two-hour rule applies. If you take calcium, take it at least two hours after your bisphosphonate - and don’t take it at the same time as magnesium. Many people take calcium and magnesium together, but that’s a problem if you’re on bisphosphonates. Space them out: bisphosphonate → wait 2 hours → then take either calcium or magnesium, but not both at once.
What if I accidentally take magnesium and my bisphosphonate together?
Don’t panic. Skip your next dose of bisphosphonate and wait until the next scheduled day. Don’t double up. Taking both together once won’t cause immediate harm, but it does reduce that day’s effectiveness. Going forward, stick to the two-hour rule. If this happens often, talk to your doctor about switching to an IV option.
Can I take magnesium at night if I take my bisphosphonate in the morning?
Absolutely. That’s actually the easiest schedule. Take your bisphosphonate at 7 AM with water. Wait until 9:30 AM to eat, then take your magnesium at dinner or before bed. That’s more than two hours apart and fits naturally into daily routines. Many patients find this the most manageable approach.




satya pradeep
November 17, 2025 AT 23:13Kelsey Robertson
November 19, 2025 AT 02:53Joseph Peel
November 20, 2025 AT 22:24Shannon Hale
November 22, 2025 AT 18:20Elia DOnald Maluleke
November 22, 2025 AT 22:59Holli Yancey
November 23, 2025 AT 21:36Prem Hungry
November 25, 2025 AT 05:06Sridhar Suvarna
November 27, 2025 AT 04:26Gordon Mcdonough
November 28, 2025 AT 14:20Bill Machi
November 29, 2025 AT 18:11