More than 1 in 4 adults in the U.S. take herbal supplements. Many of them are also on prescription drugs. What happens when these two worlds collide? The answer isn’t always obvious - and it can be dangerous.
Why Herbal Supplements Aren’t Always Safe with Medications
People often think "natural" means "safe." But that’s not true. Herbal supplements are powerful. They contain active chemicals that can change how your body handles prescription drugs. Some speed up how fast your liver breaks down medication. Others slow it down. Either way, the result can be serious.Take St. John’s wort, for example. It’s one of the most popular herbal mood boosters. But it’s also the most dangerous when mixed with other drugs. It turns on a liver enzyme called CYP3A4 - the same one that processes about half of all prescription medications. When this enzyme gets activated, drugs like birth control pills, antidepressants, blood thinners, and even HIV meds get flushed out of your system too fast. Studies show St. John’s wort can cut cyclosporine levels (used after organ transplants) by more than half. That’s not a small drop. That’s a risk of organ rejection.
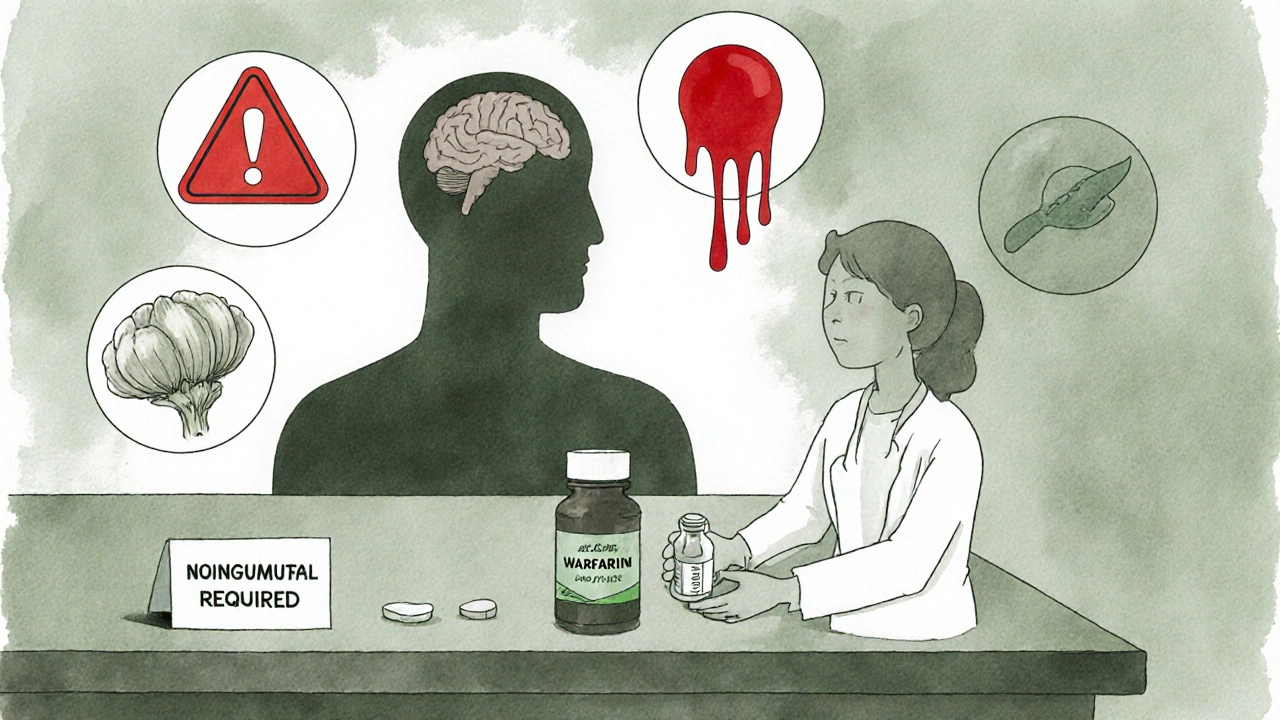
And it’s not just St. John’s wort. Garlic, goldenseal, and ginkgo biloba all interfere with drug metabolism. Garlic can reduce the effectiveness of saquinavir, an HIV drug, by over 50%. Goldenseal can make dextromethorphan (found in cough syrups) build up to toxic levels. Ginkgo can raise the risk of bleeding when taken with warfarin or aspirin.
How These Interactions Actually Happen
There are two main ways herbal supplements mess with medications: pharmacokinetic and pharmacodynamic interactions.Pharmacokinetic means the supplement changes how your body absorbs, breaks down, or gets rid of the drug. This is mostly about liver enzymes like CYP3A4 and CYP2C9, and transporters like P-glycoprotein. These are the body’s cleanup crew for drugs. If an herb like St. John’s wort turns them up to full power, your drug gets cleared too fast. If an herb like goldenseal shuts them down, your drug builds up - and that’s when toxicity kicks in.
Pharmacodynamic interactions are simpler: two things do the same thing to your body, and together they do it too well. Danshen, a Chinese herb used for heart health, thins the blood. So does warfarin. Together, they can cause dangerous bleeding. Ginseng can make blood thinners less effective by mimicking vitamin K - the very thing warfarin tries to block. One patient’s INR (a blood clotting measure) dropped from 4.9 to 1.9 after taking 1,000 mg of ginseng daily. That’s the difference between safe and life-threatening.
Top 5 High-Risk Herbal Supplements
- St. John’s wort: Interacts with at least 15 drug classes. Reduces effectiveness of birth control, antidepressants, HIV meds, transplant drugs, and heart medications. Known to cause unplanned pregnancies and transplant rejection.
- Ginkgo biloba: Increases bleeding risk with warfarin, aspirin, NSAIDs. Linked to multiple cases of brain bleeds and surgical bleeding complications.
- Garlic: Lowers levels of HIV drugs like saquinavir by over 50%. May also increase bleeding risk.
- Goldenseal: Blocks liver enzymes, raising levels of metoprolol, dextromethorphan, and other drugs. Can lead to overdose symptoms like dizziness, slowed breathing, or heart rhythm problems.
- Danshen: Increases bleeding and irregular heartbeat risk when taken with digoxin or blood thinners. One study showed a 35% higher chance of dangerous heart rhythms.
Some herbs are lower risk - like milk thistle, saw palmetto, and cranberry. But even these aren’t risk-free. Valerian can make sedatives like benzodiazepines too strong. Hawthorn can drop your blood pressure too far when taken with beta-blockers. One patient ended up in the ER after his systolic pressure fell to 85 mmHg.
Why Doctors Often Don’t Know About These Risks
A 2016 study of hospital patients found that 72% of people taking herbal supplements didn’t tell their doctors. Why? Many believe supplements are harmless. Others think their doctor doesn’t care. Or they’re embarrassed.Doctors aren’t always trained for this. A 2022 assessment showed that 62% of providers missed interactions with American ginseng. Most medical schools don’t require a single class on herbal supplements. Pharmacists at Mayo Clinic spend an average of 18 minutes counseling just one patient about St. John’s wort. That’s more time than most primary care visits last.
Even the labels don’t help. Out of 23,000 herbal products sold in the U.S. in 2022, only 15% included any warning about drug interactions. The FDA doesn’t require it. Under the 1994 Dietary Supplement Health and Education Act (DSHEA), companies don’t have to prove safety before selling. They don’t even have to test for interactions.
What You Should Do - A Simple Checklist
- Make a list of every supplement you take - including teas, tinctures, and powders. Don’t forget turmeric, ginger, or chamomile.
- Show it to your doctor every time you see them. Say: "Here’s what I’m taking besides my prescriptions." Don’t wait for them to ask.
- Ask specifically: "Could any of these interfere with my meds?" Name the drug. Ask about your most important ones: blood thinners, heart meds, antidepressants, or transplant drugs.
- Don’t start a new supplement without checking. Even something as simple as green tea extract can affect how your liver processes drugs.
- Watch for warning signs: Unexplained bruising, dizziness, irregular heartbeat, sudden changes in mood or energy, or a medication that suddenly stops working.
Visual aids help. One study found that showing patients pictures of common herbs increased disclosure by 47%. If your doctor doesn’t know what you’re taking, they can’t protect you.

The Bigger Picture: Regulation Is Broken
The global herbal supplement market hit $105 billion in 2023. People spend billions on these products believing they’re safe. But the system doesn’t work like it does for prescription drugs. There’s no pre-market safety review. No mandatory interaction testing. No real-time monitoring.The FDA issued only 12 warning letters about herb-drug risks in 2022 - despite tracking over 80,000 products. Meanwhile, researchers estimate 40-60% of dangerous interactions are never documented because patients don’t report them and doctors don’t ask.
Some progress is being made. The FDA released draft guidance in 2023 asking for interaction testing on new botanical drugs. The European Medicines Agency now requires it. The NIH spent $12.7 million in 2023 on research. AI tools are being built to predict new interactions. But none of this helps you today.
Final Thought: Natural Doesn’t Mean Harmless
Herbal supplements are medicine. They’re not candy. They’re not just "helping your body heal." They’re chemically active. And when mixed with prescription drugs, they can turn a safe treatment into a life-threatening situation.St. John’s wort isn’t the only problem. Ginkgo, garlic, goldenseal, danshen - they’re all real risks. And they’re all easy to miss.
If you’re on any medication - especially for heart disease, mental health, blood thinning, or organ transplants - assume your herbal supplement could interfere. Talk to your doctor. Show them your bottle. Ask the question. Your life might depend on it.
Can herbal supplements really make my prescription drugs stop working?
Yes. St. John’s wort is the most well-documented example. It can reduce the effectiveness of birth control pills, antidepressants, HIV medications, and transplant drugs by up to 80%. This isn’t speculation - it’s been proven in clinical studies. A transplant patient taking St. John’s wort saw cyclosporine levels drop by 57%, putting their new organ at risk of rejection. Even over-the-counter drugs like warfarin can become less effective when mixed with ginseng.
I take turmeric for inflammation. Is that safe with my blood pressure meds?
Turmeric itself has low interaction risk, but many turmeric supplements contain black pepper extract (piperine) to boost absorption. Piperine can slow down how your liver breaks down some blood pressure drugs, leading to higher levels in your blood. This can cause dizziness, low heart rate, or even fainting. Always check the full ingredient list - not just the main herb.
Why don’t supplement labels warn about drug interactions?
Because they’re not required to. Under U.S. law (DSHEA, 1994), dietary supplements don’t need FDA approval before being sold. Companies don’t have to prove safety, effectiveness, or interaction risks. Only about 15% of herbal products include interaction warnings, even though 62% of users take them with prescription drugs. The system is built on trust - not science.
I’m on warfarin. What herbs should I absolutely avoid?
Avoid ginkgo biloba, garlic, danshen, ginger, and ginseng. These can all increase your bleeding risk. Ginkgo alone has been linked to over 30 documented cases of serious bleeding in patients on warfarin. Even green tea and cranberry juice - often thought as harmless - can affect how warfarin works. Your INR levels can swing unpredictably. Always tell your doctor what you’re taking, and get your blood tested regularly.
My doctor says supplements are fine. Should I still worry?
Many doctors simply don’t know the full risks. A 2024 study found only 3% of primary care providers routinely screen for herb-drug interactions. If your doctor says it’s fine, ask: "Is there any research showing this is safe with my specific medications?" If they can’t point to a study, don’t assume safety. Keep your own records and bring them to every appointment.
Next Steps: Protect Yourself
Start today. Write down every supplement you take - even the ones you think are "just for relaxation" or "mildly helpful." Then, schedule a 10-minute chat with your doctor or pharmacist. Bring your bottles or a photo of the labels. Ask: "Could any of these interfere with my medications?" Don’t wait for a problem to happen. Prevention is the only reliable defense.Herbal supplements aren’t the enemy. But treating them like harmless tea is dangerous. When you combine them with prescription drugs, you’re playing with chemistry - and the stakes are your health.




kaushik dutta
November 29, 2025 AT 06:30Let me be blunt-this post nails it. In India, we’ve got grandmas popping St. John’s wort with antihypertensives and calling it ‘Ayurvedic balance.’ No one checks CYP3A4 kinetics. No one. The FDA’s toothless under DSHEA, and pharma’s too busy lobbying to care. We need mandatory interaction labeling-like cigarette warnings. Not suggestions. Mandates. This isn’t wellness. It’s pharmacokinetic roulette.
Olivia Gracelynn Starsmith
November 30, 2025 AT 08:01Thank you for laying this out so clearly. I’ve been taking turmeric for years and never knew the piperine in black pepper could affect my blood pressure meds. I’ll bring my supplement bottle to my next appointment and ask specifically about interactions. It’s easy to assume natural equals safe, but this is a wake-up call. I’m grateful for the checklist.
Skye Hamilton
November 30, 2025 AT 13:57ok so like… what if i told you the real villain isn’t herbs… it’s the FDA… and the pharmaceutical industry… they dont want you to know that nature has better medicine… and they profit off your dependency on synthetics… also ginkgo is fine if you dont take warfarin… but they scare you so you keep buying pills…
Maria Romina Aguilar
December 1, 2025 AT 04:51I’ve been reading this article, and I just… I don’t know. I mean, I’ve been taking garlic capsules for five years, and my blood pressure is better than ever. And now you’re telling me it could be dangerous? I feel like I’ve been lied to. And I’m not even sure I believe the study about saquinavir. It just seems… too convenient. Like someone wants us to stop using natural remedies.
Brandon Trevino
December 2, 2025 AT 17:46Statistical literacy is absent in public discourse. 72% of patients conceal supplement use-this is not anecdotal. It is epidemiological. The CYP3A4 induction by hypericum perforatum is documented in NEJM, Lancet, JAMA. The FDA’s 12 warning letters in 2022 reflect systemic under-enforcement, not absence of risk. The 1994 DSHEA loophole is a regulatory failure of historic proportion. This is not fearmongering. It is pharmacovigilance.
Denise Wiley
December 3, 2025 AT 07:20OMG I JUST REALIZED I’VE BEEN TAKING GINSENG WITH MY ANTIDEPRESSANTS FOR MONTHS 😱 I’M SO GLAD I READ THIS. I’VE BEEN FEELING WEIRD AND TIRED AND THOUGHT IT WAS JUST STRESS. I’M GOING TO STOP IT TONIGHT AND CALL MY DOCTOR TOMORROW. THANK YOU FOR THIS. WE NEED MORE POSTS LIKE THIS. SERIOUSLY.
Hannah Magera
December 3, 2025 AT 19:18I didn’t know any of this. I just thought supplements were like vitamins. I take chamomile tea every night and assumed it was harmless. I’ll start writing down everything I take and ask my doctor. I feel like I’ve been careless. Thanks for making it simple to understand.
Austin Simko
December 3, 2025 AT 21:24They’re watching you. The FDA. Big Pharma. They’re putting toxins in your supplements to make you sick so they can sell you more drugs. They don’t want you to heal naturally. That’s why they don’t test interactions. They want you dependent.
Nicola Mari
December 5, 2025 AT 20:29It is appalling that people treat their bodies like a chemistry experiment without consulting a professional. You are not a self-diagnosed wellness influencer. You are not a pharmacist. You are not qualified. And yet you consume these substances as if they were candy. The consequences are not hypothetical. They are documented. And you are responsible. Shame on you.
Sam txf
December 6, 2025 AT 03:36St. John’s wort is a goddamn weapon. I’ve seen it take down a transplant patient’s cyclosporine levels like a sniper. And yeah, the FDA’s asleep at the wheel. But here’s the real truth: people don’t want to be told no. They want their herbal tea and their antidepressants and their magic pills. They want the fantasy. So they lie to their doctors. And then they wonder why they end up in the ER. It’s not the herb. It’s the arrogance.
George Hook
December 7, 2025 AT 21:04I’ve been a pharmacist for 22 years, and I can tell you this: the biggest issue isn’t the herbs themselves-it’s the lack of communication. I’ve had patients come in with 17 different supplements, none of which they mentioned during their intake. One woman was on warfarin, ginkgo, garlic, and turmeric-all without telling her cardiologist. Her INR was 8.4. She nearly bled out. We saved her, but she didn’t need to be in that position. It’s not about scaring people. It’s about empowering them with knowledge. I wish every patient brought their supplements in a baggie. I’d have fewer nightmares.
jaya sreeraagam
December 8, 2025 AT 20:34As someone who grew up in a family that used herbal remedies daily, I want to say thank you for validating our culture while also warning us. My grandmother used danshen for heart health-she didn’t know it could interfere with digoxin. I’ve started creating a simple chart for my relatives: herb, drug, risk, what to do. I’m sharing it on WhatsApp groups. We need to bridge tradition and science-not fight them. Education is the bridge, not judgment. And yes, I typed this on my phone, so forgive the typos-I’m trying to reach people who don’t read long articles.
Katrina Sofiya
December 9, 2025 AT 12:45This is an exceptionally well-researched and vital piece of public health communication. The integration of clinical evidence, regulatory context, and actionable guidance is masterful. I have shared this with my entire primary care network, and I encourage all healthcare professionals to incorporate this checklist into their intake protocols. The burden of safety should not fall solely on the patient. Systemic change begins with awareness-and this post is a catalyst.
doug schlenker
December 9, 2025 AT 21:18I used to think this stuff was just hype. But my cousin’s mom had a brain bleed after starting ginkgo with aspirin. She was 72, healthy, thought it was just for memory. No one told her. I read this and felt sick. I’m going to sit down with my dad-he’s on blood pressure meds and takes turmeric and ginger. I’ll bring the bottle. I don’t want to lose him because we didn’t ask the right questions. Thanks for saying what needed to be said.
Denise Wiley
December 10, 2025 AT 03:25OMG I JUST REALIZED I’VE BEEN TAKING GINSENG WITH MY ANTIDEPRESSANTS FOR MONTHS 😱 I’M SO GLAD I READ THIS. I’VE BEEN FEELING WEIRD AND TIRED AND THOUGHT IT WAS JUST STRESS. I’M GOING TO STOP IT TONIGHT AND CALL MY DOCTOR TOMORROW. THANK YOU FOR THIS. WE NEED MORE POSTS LIKE THIS. SERIOUSLY.