What Really Causes Constipation?
Constipation isn’t just about not going to the bathroom often. Medically, it’s defined as having fewer than three bowel movements a week, with hard, dry stools that are hard to pass. It’s not rare-about one in three people in clinical settings deal with it regularly. In the U.S. alone, over 2.5 million people visit doctors each year just for this issue.
The problem usually starts when your colon absorbs too much water from waste. Normally, food moves through your digestive tract in 24 to 72 hours. But when it slows down, stool becomes dry and packed, making it tough to push out. This isn’t always about diet. It can come from how your muscles work, what meds you’re on, or even underlying health conditions.
Types of Constipation You Might Not Know About
Not all constipation is the same. Doctors break it into four main types, and knowing which one you have changes how you treat it.
- Normal transit constipation (60% of cases): Your stool moves through your colon at a normal speed, but you still feel like you’re straining, not fully emptying, or passing hard pellets. This is often tied to pelvic floor issues or poor toilet habits.
- Slow transit constipation (15-30%): Your colon is sluggish. Stool takes more than 72 hours to move through. This is more common in women and older adults.
- Defecatory disorders (20-50%): Your pelvic floor muscles don’t relax properly when you try to poop. Instead of pushing stool out, they clench. You might feel like you’re pushing but nothing comes out. A simple test-trying to push out a water-filled balloon in under a minute-can spot this.
- Refractory constipation (15-20%): You’ve tried multiple laxatives and nothing works. This often needs specialist care.
Medications That Can Cause Constipation
It’s easy to blame your diet, but sometimes the culprit is something you’re taking every day.
- Opioids (painkillers like oxycodone or morphine): Up to 95% of people on long-term opioids get constipated.
- Calcium channel blockers (for high blood pressure): Drugs like nifedipine or verapamil slow gut movement in 10-20% of users.
- Tricyclic antidepressants: These older depression meds affect nerves in the gut, causing constipation in 20-30% of people.
- Iron supplements: Common in women and older adults, iron is notorious for hardening stool.
If you started a new medication and noticed changes in your bowel habits, talk to your doctor before stopping anything. Sometimes switching to a different drug helps.
Medical Conditions Linked to Constipation
Constipation doesn’t happen in a vacuum. It’s often a sign of something deeper.
- Diabetes: Nearly 60% of people with diabetes experience constipation. High blood sugar damages the nerves that control gut movement.
- Hypothyroidism: When your thyroid is underactive, your whole metabolism slows-including your bowels. About 10-15% of constipation cases link back to this.
- Neurological diseases: Parkinson’s affects 50-80% of patients. Multiple sclerosis hits 30-50%. Spinal cord injuries? Up to 80% struggle with bowel control.
- Stroke or paralysis: Reduced mobility and nerve damage make bowel function unpredictable.
Women are more likely to have constipation than men-33% vs. lower rates in men. And the older you get, the worse it gets. After age 60, prevalence rises by about 1.5% each year.
How Laxatives Actually Work (And Which Ones to Use)
Laxatives aren’t all the same. Each type works differently-and some are better for long-term use than others.
- Bulk-forming laxatives (psyllium, methylcellulose): These soak up water like a sponge, swelling into soft, bulky stool that triggers natural contractions. They’re great for normal transit constipation, but you must drink enough water. Without it, they can cause blockages. Take at least 8 ounces of water with each dose.
- Osmotic laxatives (PEG 3350, lactulose, magnesium hydroxide): These pull water into your colon, softening stool. PEG 3350 (Miralax) is the gold standard. Studies show 65-75% of people respond well, with minimal side effects. It’s safe for daily use, even long-term.
- Stimulant laxatives (senna, bisacodyl): These force your intestines to contract. They work fast-usually within 6-12 hours. But using them for more than 2-3 weeks can damage your colon’s natural rhythm. Long-term use can lead to “cathartic colon,” where your gut stops working on its own.
- Stool softeners (docusate sodium): These are often overhyped. Studies show they’re barely better than a placebo. Don’t rely on them alone.
For stubborn cases, doctors may prescribe:
- Lubiprostone (Amitiza): Activates chloride channels to increase fluid in the gut. Works in 40-50% of patients.
- Linaclotide (Linzess) and plecanatide (Trulance): These mimic natural gut hormones to boost fluid secretion. Response rates are 45-60%.
- Tenapanor (Ibsrela): Approved in 2022, it blocks sodium absorption in the gut, reducing water loss and softening stool.
Long-Term Management: Beyond Pills
If you’ve been using laxatives for months and still feel stuck, it’s time to look beyond pills. Real, lasting relief comes from lifestyle changes.
1. Fiber-But Do It Right
The recommended daily fiber intake is 25-30 grams. Most people get only 15. But don’t jump to 30g overnight. Adding more than 5g per day too fast causes bloating in 30-40% of people. Increase slowly: add 5g every 3-4 days. Focus on soluble fiber-oats, beans, apples, chia seeds. It holds water and makes stool softer.
2. Hydration Matters More Than You Think
For every 5g of extra fiber you add, drink an extra 250-500mL of water. If you’re taking 25g of psyllium, you need at least 2.5 liters of water daily. Dehydration turns fiber into cement.
3. Train Your Body to Go
Your body responds to routine. Sit on the toilet for 10-15 minutes after breakfast. That’s when your gastrocolic reflex is strongest-your colon naturally contracts after eating. Don’t rush. Don’t strain. Just sit.
4. Fix Your Position
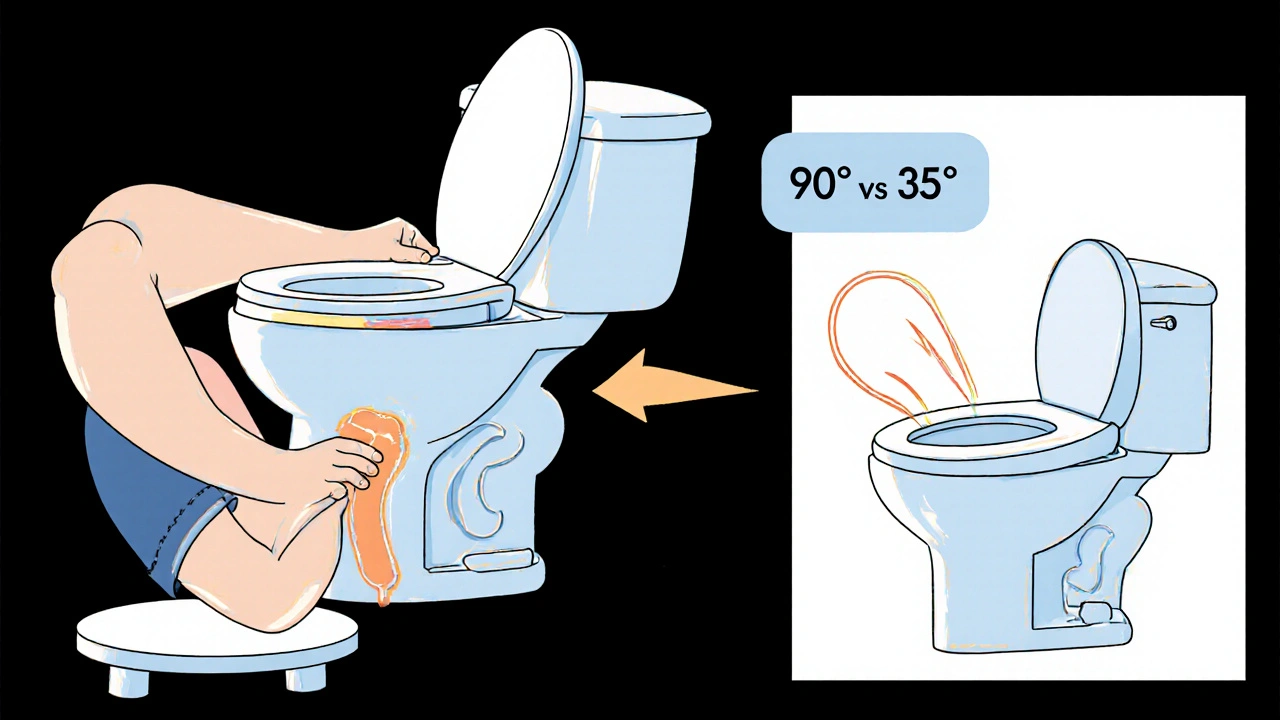
Sitting on a modern toilet puts your colon at a 90-degree angle. That’s not natural. Squatting straightens the path. Use a footstool to raise your feet. This creates a 35-degree hip flexion-studies show it reduces straining by 60%.
5. Try Biofeedback
If you have a defecatory disorder, your muscles aren’t working right. Biofeedback therapy uses sensors to show you how your pelvic floor moves. With 6-8 weekly sessions, 70-80% of people learn to relax the right muscles. It’s not cheap ($100-$150 per session), but it’s one of the most effective long-term fixes.
When to Worry: Alarm Symptoms
Constipation is usually harmless. But sometimes, it’s a red flag.
See a doctor right away if you have:
- Unintentional weight loss of 10 pounds or more
- Rectal bleeding
- Bowel habits that change for more than 6 weeks
- A family history of colorectal cancer
These aren’t normal. They could signal tumors, inflammatory disease, or other serious conditions.

Why Most People Fail at Long-Term Relief
Here’s the hard truth: 68% of people who start a fiber and water plan relapse within 3 months. Why? They give up too soon. It takes 4-6 weeks for your gut to adjust. And 35% of patients say their doctor gave them less than 5 minutes of advice.
Another problem? Expectations. People think laxatives should work in 24 hours. But osmotic ones like PEG take 48-72 hours. If you don’t know that, you’ll keep doubling your dose-and end up with diarrhea.
And then there’s the myth of “laxative dependency.” Laxatives don’t make your colon lazy. But if you rely on stimulants for years, your body can lose its natural rhythm. That’s why guidelines say: avoid stimulants longer than 3 months.
What Works in Real Life
One woman, 52, had chronic constipation for 15 years. She tried everything: senna, magnesium, enemas. Nothing stuck. Then she changed three things:
- 25g of psyllium husk every morning with 2L of water
- 10 minutes of squatting on a footstool after breakfast
- Drinking coffee-its caffeine triggers the gastrocolic reflex
Within 8 weeks, she had regular, easy bowel movements. No pills. No side effects.
On Reddit’s r/Constipation community, 70% of users who tried magnesium citrate (250-350mg daily) said it worked. But 25% got diarrhea. So start low.
The Bigger Picture
Constipation costs the U.S. over $1.7 billion a year. The global laxative market hit $2.3 billion in 2022. But the real cost is quality of life. People miss work. They avoid social events. They feel embarrassed.
Future treatments are coming. Researchers are mapping gut bacteria linked to constipation-Bacteroides uniformis is often missing. AI tools are being developed to analyze squatting posture via smartphone apps, catching pelvic floor issues early.
But the most powerful tool right now? Knowledge. Knowing when to use fiber, when to drink more water, when to see a specialist. You don’t need to suffer. You just need the right plan.
How long does it take for laxatives to work?
It depends on the type. Stimulant laxatives like senna usually work in 6-12 hours. Osmotic laxatives like PEG 3350 take 1-3 days. Bulk-forming laxatives may take 2-3 days to build up. Don’t expect overnight results-especially with fiber and hydration changes. Patience is key.
Can constipation be cured without medication?
Yes, for many people. Up to 60% of chronic constipation cases are normal transit constipation, which responds well to fiber, water, posture, and routine. Biofeedback therapy helps 70-80% of people with pelvic floor dysfunction. Lifestyle changes aren’t just alternatives-they’re the foundation of long-term relief.
Is it safe to take laxatives every day?
Osmotic laxatives like PEG 3350 are safe for daily, long-term use. Stimulant laxatives like senna are not. Using them for more than 3 months can damage your colon’s natural ability to contract. Always start with the mildest option and only move up if needed. Talk to your doctor before using any laxative daily.
Why do I still feel constipated even though I eat fiber?
You might not be drinking enough water. Fiber needs water to swell and soften stool. If you add fiber but stay dehydrated, your stool gets harder. Also, if you’re eating insoluble fiber (like bran) without soluble fiber (like oats or beans), it can cause bloating without improving movement. Try a mix-2/3 soluble, 1/3 insoluble.
When should I see a doctor for constipation?
See a doctor if you’ve had symptoms for more than 3 weeks despite lifestyle changes, or if you have warning signs: unexplained weight loss, rectal bleeding, vomiting, severe abdominal pain, or a family history of colon cancer. Also, if you’re over 50 and constipation is new, get checked. It’s not always just diet.


Jennifer Walton
November 15, 2025 AT 16:12Kihya Beitz
November 16, 2025 AT 14:19John Foster
November 18, 2025 AT 06:50Edward Ward
November 19, 2025 AT 03:49Andrew Eppich
November 20, 2025 AT 17:43Adam Dille
November 20, 2025 AT 19:58Katie Baker
November 21, 2025 AT 05:34Jessica Chambers
November 22, 2025 AT 04:46Shyamal Spadoni
November 24, 2025 AT 01:05Ogonna Igbo
November 24, 2025 AT 04:35BABA SABKA
November 25, 2025 AT 04:12Chris Bryan
November 25, 2025 AT 22:32Jonathan Dobey
November 26, 2025 AT 18:15