Osteoporosis Medications: What Works, What to Watch For
When your bones start losing density, osteoporosis medications, drugs designed to slow bone loss and reduce fracture risk. Also known as bone-strengthening drugs, they’re not just pills for older people—they’re essential tools for anyone with low bone mass, a history of fractures, or high risk from conditions like rheumatoid arthritis or long-term steroid use. These aren’t magic bullets, but they do work when used right. The goal isn’t to make bones young again, but to stop them from breaking too easily.
There are a few main types of bisphosphonates, oral or IV drugs that block cells that break down bone. Also known as bone resorption inhibitors, they include alendronate (Fosamax), risedronate (Actonel), and zoledronic acid (Reclast). These are often the first choice because they’re well-studied, affordable, and cut fracture risk by up to 50% in the spine. But they’re not for everyone. Some people can’t swallow them, others get stomach upset, and a rare but serious side effect is jawbone damage. Then there’s denosumab, a monthly injection that works differently by targeting a specific protein that triggers bone loss. Also known as RANK ligand inhibitor, it’s strong, effective, and often used when bisphosphonates fail or aren’t tolerated. But if you stop it, bone loss can rush back—so you can’t just quit cold turkey.
For people with severe osteoporosis or those who’ve broken bones despite other treatments, teriparatide, a daily injection that actually builds new bone instead of just slowing loss. Also known as PTH analog, it’s the only osteoporosis drug that stimulates bone formation. It’s expensive, requires daily shots for up to two years, and isn’t meant for long-term use. After that, most people switch to a bisphosphonate or denosumab to hold onto the gains. There’s also abaloparatide and romosozumab—newer options with similar effects but different risks. All of them need careful monitoring. You can’t just take these pills and forget about it. You still need calcium, vitamin D, weight-bearing exercise, and fall prevention. These drugs work best when paired with lifestyle changes.
The posts below cover real-world details you won’t get from a drug label: how to track if your medication is working, what to do if you miss a dose, how to handle side effects like jaw pain or muscle cramps, and why some people switch from one drug to another. You’ll find guides on comparing options, managing interactions with other meds, and what to ask your doctor before starting—or stopping—any of these treatments. No fluff. No marketing. Just what you need to know to stay safe and strong.
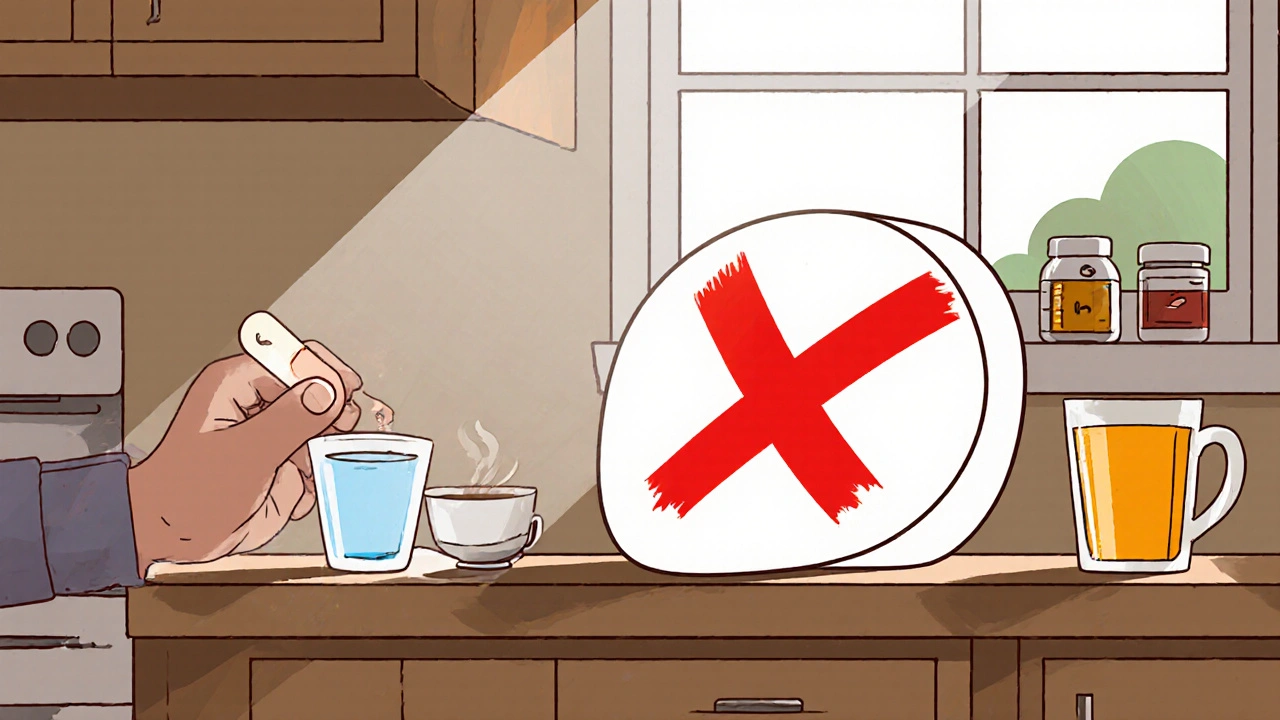
Magnesium Supplements and Osteoporosis Medications: Timing Rules
Magnesium supplements can block osteoporosis medications like Fosamax and Actonel, reducing their effectiveness by up to 60%. Follow a strict 2-hour timing rule to protect your bones and prevent fractures.
November 17 2025