Bisphosphonates: What They Are, How They Work, and What You Need to Know
When your bones start losing density faster than they can rebuild, bisphosphonates, a class of drugs designed to slow bone breakdown and preserve bone mass. Also known as bone-resorption inhibitors, they’re one of the most prescribed treatments for osteoporosis and other conditions that weaken the skeleton. If you’ve been told you have low bone mass or a history of fractures, chances are bisphosphonates came up in your conversation with your doctor. But what exactly do they do—and are they right for you?
Bisphosphonates work by targeting cells called osteoclasts, which break down old bone tissue. In healthy people, this process is balanced by osteoblasts, the cells that build new bone. But as we age, or with conditions like menopause or long-term steroid use, osteoclasts get too active. Bisphosphonates stick to the bone surface and quiet down these overactive cells, helping bone density stay stable—or even improve slightly over time. That’s why they’re used not just for osteoporosis, but also for bone metastases, Paget’s disease, and even rare conditions like osteogenesis imperfecta. They don’t rebuild bone like magic; they just stop it from falling apart too fast.
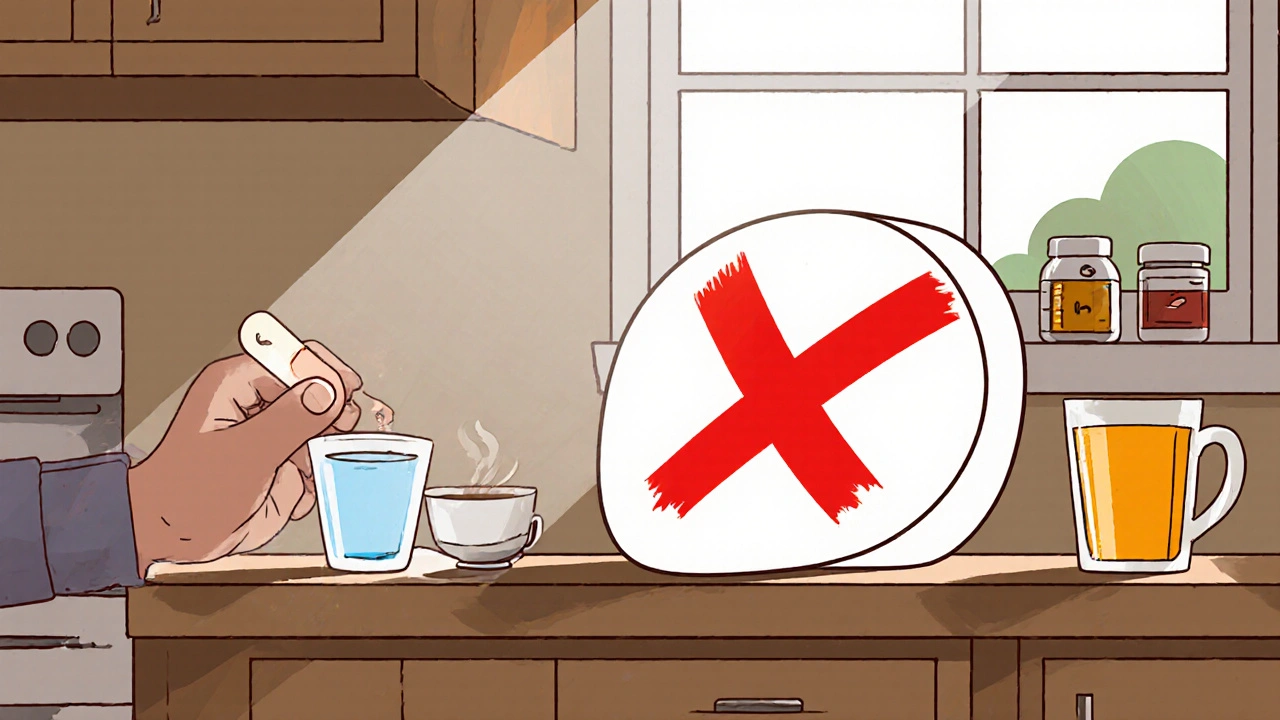
Not all bisphosphonates are the same. Some, like alendronate (Fosamax), are taken weekly as a pill. Others, like zoledronic acid (Reclast), come as a once-a-year IV infusion. The choice depends on your health, how well you can stick to a dosing schedule, and whether your stomach can handle oral versions. You might hear about jaw problems or unusual thigh fractures linked to long-term use—but these are rare. Most people take them safely for years without issues, especially when they follow the simple rules: take them on an empty stomach with a full glass of water, stay upright for 30 minutes, and don’t lie down right after.
These drugs don’t work in isolation. They’re part of a bigger picture that includes vitamin D, calcium intake, weight-bearing exercise, and avoiding smoking or heavy alcohol. If you’re on a bisphosphonate, you’re not just taking a pill—you’re managing your bone health over time. That’s why tracking your bone density scans and talking to your doctor about when to pause or switch treatments matters. Some people take them for 3–5 years, then take a break. Others need them longer. There’s no one-size-fits-all plan.
You’ll find posts here that dig into how bisphosphonates compare with other bone drugs, what to do if you miss a dose, how they interact with other meds like proton-pump inhibitors, and why some people stop taking them because of side effects like heartburn or muscle pain. You’ll also see real-world advice on staying safe while using them, how to monitor for rare complications, and what alternatives exist if they don’t work for you. This isn’t just about pills—it’s about keeping your bones strong enough to live the life you want, without fear of a fall turning into a fracture.
Magnesium Supplements and Osteoporosis Medications: Timing Rules
Magnesium supplements can block osteoporosis medications like Fosamax and Actonel, reducing their effectiveness by up to 60%. Follow a strict 2-hour timing rule to protect your bones and prevent fractures.
November 17 2025