Glaucoma isn’t just high eye pressure. It’s a silent thief of vision, quietly damaging the optic nerve long before you notice anything wrong. Most people don’t feel pain, don’t see blurriness, and don’t realize their peripheral vision is fading-until it’s too late. That’s why glaucoma is the second leading cause of blindness worldwide, affecting over 76 million people today, with numbers expected to hit nearly 112 million by 2040. The real danger? You can have normal eye pressure and still develop glaucoma. Or you can have high pressure and never lose sight. The key isn’t just the number on the tonometer-it’s what’s happening at the back of your eye.
What Really Happens in Glaucoma?
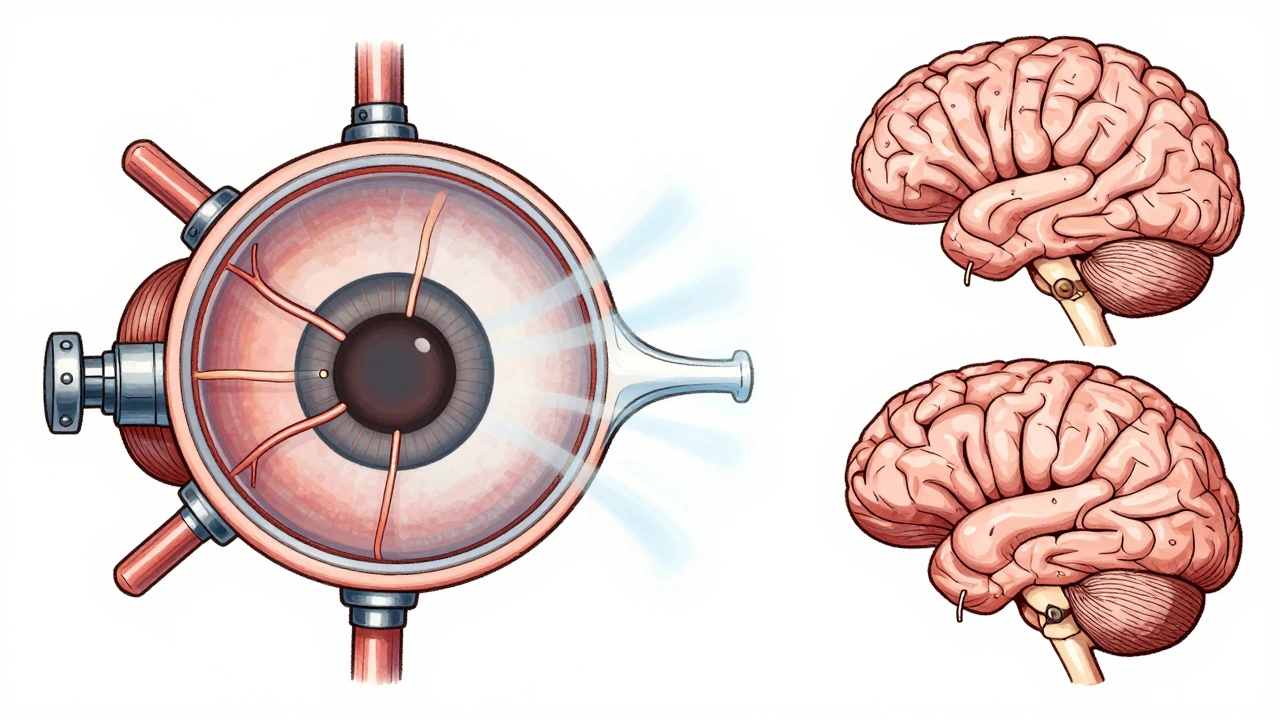
The optic nerve is the cable that carries every visual signal from your eye to your brain. In glaucoma, this nerve gets damaged. For decades, doctors thought elevated eye pressure-called intraocular pressure or IOP-was the main culprit. And while high IOP is a major risk factor, it’s not the whole story. Modern research shows that pressure at the optic nerve head, where the nerve exits the eye, causes mechanical strain on a delicate mesh-like structure called the lamina cribrosa. Think of it like a sieve under stress: when pressure pushes against it, the tiny tunnels that carry nerve fibers get stretched and crushed. Over time, this kills the retinal ganglion cells that make up the optic nerve.
Normal IOP ranges between 10 and 21 mmHg, measured with the gold-standard Goldmann applanation tonometer. But pressure isn’t constant. It rises naturally in the early morning, often peaking between 6 and 8 a.m. That’s why some people with normal daytime readings still have glaucoma progression. What matters more than a single number is the pressure difference between the inside of your eye and the pressure in your brain. Studies show that people with glaucoma often have lower cerebrospinal fluid pressure than healthy individuals. That means even if your eye pressure is 18 mmHg, if your brain pressure is only 9 mmHg, the net force pushing on your optic nerve is 9 mmHg-a dangerous gap. In contrast, people with ocular hypertension (high pressure but no nerve damage) often have higher brain pressure, which protects the nerve.
Types of Glaucoma: It’s Not One Disease
Glaucoma comes in several forms, each with different causes and risks. About 90% of cases in the U.S. are primary open-angle glaucoma (POAG). It develops slowly, with no symptoms, and the drainage angle of the eye remains open but becomes clogged over time. Normal-tension glaucoma (NTG) affects 20-30% of people in Western countries and up to 70% in parts of Asia. These patients have IOP consistently below 21 mmHg, yet their optic nerves still deteriorate. Why? The damage may come from poor blood flow to the nerve, genetic factors, or a vulnerability in the lamina cribrosa. Then there’s angle-closure glaucoma, which is less common globally but responsible for half of all glaucoma-related blindness in Asia. This type happens when the iris blocks the drainage angle suddenly, causing a rapid, painful pressure spike that needs emergency treatment.
Secondary glaucomas-like pseudoexfoliative or pigmentary glaucoma-make up about 10% of cases. They’re caused by other conditions, like eye inflammation, trauma, or cataracts. These often progress faster and require more aggressive treatment.
How Doctors Diagnose Glaucoma
There’s no single test. Diagnosis relies on three key tools working together. First, optical coherence tomography (OCT) scans the retina and measures the thickness of the retinal nerve fiber layer. It can detect thinning as small as 5-10 microns-thinner than a human hair-before vision loss occurs. Second, visual field testing, usually with Humphrey perimetry, maps your peripheral vision. It identifies tiny blind spots as small as 1 dB in sensitivity. Third, fundus photography captures the appearance of the optic disc. A deepening cup or asymmetry between eyes signals damage.
These tests are repeated regularly. The American Academy of Ophthalmology recommends annual visual field tests and OCT scans every 6 to 12 months for people with diagnosed glaucoma. IOP checks happen every 3 to 6 months. Many patients find the visual field test tedious-it takes 30 minutes per eye, and you have to press a button every time you see a flash of light. But skipping it risks missing progression.
Treatment: Lowering Pressure Isn’t Enough-But It’s Still the Best Start
Reducing IOP remains the only proven way to slow glaucoma. The Early Manifest Glaucoma Trial showed that lowering pressure by 25-30% cuts progression risk by half. Target pressure depends on how advanced the disease is. For mild cases, doctors aim for a 20-25% reduction from baseline. For severe cases, they push for 30-50% lower, sometimes to 12-15 mmHg.
First-line treatment is almost always prostaglandin analogs like latanoprost. These drops work by increasing fluid drainage from the eye. They’re taken once a day, usually at night, and reduce IOP by 25-33%. But they come with side effects: eyelashes grow longer and darker, eyelids can darken, and fat around the eye may shrink-changing your appearance over time. About 20-30% of patients stop using them because of this.
Laser treatment, called selective laser trabeculoplasty (SLT), is the next step for many. It improves drainage without cutting. It works in 75% of patients, lowering pressure by 20-30%. But its effect fades over time-about 10% per year. If drops and lasers fail, surgery is next. Trabeculectomy creates a new drainage channel. It’s successful in 85-90% of cases after one year, but about a third of patients need additional procedures by five years. Newer minimally invasive glaucoma surgeries (MIGS), like iStent, are safer and have fewer complications, reducing pressure by 20-25% with a 70-80% success rate over two years.
The Hidden Struggle: Adherence and Anxiety
Glaucoma treatment is a lifelong commitment. But nearly half of patients stop taking their drops within a year. Reasons? Side effects, forgetfulness, cost (medication averages $1,200-$1,800 a year in the U.S.), and the fact that they feel fine. One Reddit user wrote: “My IOP has been 12-13 for five years, and my vision is still getting worse.” That’s the cruel reality of normal-tension glaucoma-pressure isn’t the whole story.
Another hidden burden is fear. A 2022 survey of 1,200 patients found 68% lived with constant anxiety about going blind. Even with treatment, the uncertainty lingers. That’s why some patients find comfort in newer tools like home tonometry. Devices like the Triggerfish contact lens sensor monitor pressure changes throughout the day, giving a clearer picture than a single office visit. And AI-powered OCT analysis can now detect early glaucoma with 94% accuracy, catching changes before the patient even notices.

What’s Next? Beyond Pressure
Scientists are no longer focused only on pressure. Research is now exploring ways to protect the nerve itself. In animal studies, a protein called oncomodulin triggered 40% regeneration of damaged optic nerve fibers. The LIBERTI trial showed that brimonidine, a glaucoma drop, slowed progression in normal-tension glaucoma even more than other drops-suggesting it may have direct neuroprotective effects. Clinical trials are now testing CNTF implants, gene therapies to improve drainage, and stem cells to rebuild damaged nerve tissue.
But here’s the hard truth: we still don’t fully understand why some people’s nerves break down under pressure while others don’t. The real targets of damage aren’t just the nerve fibers-they’re the supporting cells around them: astrocytes, microglia, and the blood vessels that feed the nerve. Fixing glaucoma won’t just mean lowering pressure. It will mean protecting the nerve’s entire ecosystem.
What You Can Do
If you’re over 40, get a comprehensive eye exam-even if you see fine. Glaucoma doesn’t wait for symptoms. If you have a family history, diabetes, or are of African, Hispanic, or Asian descent, you’re at higher risk. Stick to your drops. Don’t skip tests. Ask your doctor about your target pressure and what your OCT scans show. If you’re worried about side effects, talk to them-there are alternatives. And if you’re feeling anxious, you’re not alone. Glaucoma is manageable, not a death sentence. With early detection and consistent care, most people keep their vision for life.


Ada Maklagina
December 5, 2025 AT 16:07Been on latanoprost for 3 years. Lashes are wild now. Like a raccoon tried to nest in my eyelids. Also my left eyelid looks like it lost a bet. But I can still see the streetlights at night. Worth it.
Norene Fulwiler
December 7, 2025 AT 04:01I used to think glaucoma was just old people stuff. Then my mom lost half her vision in one eye and the doctor said "it’s been creeping for years." We didn’t even know she was at risk. If you’re over 40, get checked. Even if you think you’re fine. Your eyes don’t scream until it’s too late.
And yeah, the drops are a pain. The cost? Brutal. But skipping them? That’s playing Russian roulette with your sight. I wish someone had told me this sooner.
James Moore
December 8, 2025 AT 09:36Let me just say this-modern medicine has turned glaucoma into a corporate profit machine. Drops that cost $1,500 a year? Laser treatments that "work" for a year and then fizzle? And don’t get me started on OCT scans-$300 a pop, and they’re just fancy digital snapshots of your eyeball! Meanwhile, the real solution? Lifestyle. Diet. Sleep. Blood pressure. Stress. But no, we’d rather pump your eye full of chemicals and bill your insurance for it. The system is broken. You’re being sold a lie that pressure is the villain. It’s not. It’s the system.
And yes, I’ve read the studies. I’ve seen the papers. And I’ve watched my uncle go blind while his doctor kept pushing more drops. He didn’t need more drops. He needed better sleep, less sugar, and less stress. But the system doesn’t care. It just wants your co-pay.
Harry Nguyen
December 9, 2025 AT 04:54So let me get this straight-we’re spending billions on eye drops and lasers while people in other countries are getting cured by yoga and chanting? And you’re telling me this isn’t just a scam to keep pharma rich? I’ve seen videos of people in India reversing glaucoma with eye exercises. No drugs. No lasers. Just discipline. But nope, we’d rather pay $1,800 a year for a drop that makes your eyelashes look like a Halloween prop. Pathetic.
Katie Allan
December 9, 2025 AT 21:13Thank you for writing this with such care. I’ve been living with normal-tension glaucoma for 8 years, and I’ve never met anyone who truly understood how lonely it feels. You don’t look sick. You don’t feel sick. But you’re terrified every time you forget your drops. Every time your vision feels a little fuzzier. Every time you wonder if this is the year it all slips away.
It’s not just about pressure. It’s about being seen. About knowing someone else gets it. You’re not alone. And you’re not failing. You’re fighting. And that matters more than any IOP number.
Deborah Jacobs
December 11, 2025 AT 04:26My aunt’s optic nerve looked like a crumpled paper towel after a storm. OCT showed she’d lost 40% of her nerve fibers before she ever noticed a blind spot. She’s 62, vegan, hikes every weekend, and still got hit. No family history. No high pressure. Just… bad luck? Or bad biology?
It’s wild how the body can betray you without a warning siren. I started getting annual OCTs after she lost her peripheral vision. I’m not scared-I’m vigilant. I’ve got my drops on my phone’s alarm. I’ve got my visual field test scheduled like a yoga class. This isn’t just medicine. It’s survival theater. And I’m showing up.
Also-brimonidine made my eyelids feel like they were wrapped in velvet. Like my eyes were hugging me back. Weird. But nice. And no lash growth. So I’m sticking with it.
Manish Shankar
December 12, 2025 AT 03:27As a physician in Mumbai, I treat many patients with normal-tension glaucoma. In our population, it is far more prevalent than in the West. Many patients present with advanced disease because they do not have access to regular screening. Even when they do, the cost of medications and follow-up imaging is prohibitive.
I have seen patients who, despite having IOP below 15 mmHg, show rapid progression due to vascular insufficiency and genetic predisposition. We are beginning to study the role of endothelial dysfunction and microcirculation in the optic nerve head. This is not merely a pressure issue-it is a vascular and neurodegenerative condition.
Our challenge is not just treatment, but equity. A drop that costs $1,800 in the U.S. costs less than $5 in India-but it is still unaffordable for many. We need global solutions, not just technological ones.
luke newton
December 12, 2025 AT 03:34You people are pathetic. You’re all just scared little sheep taking your little drops because the doctors told you to. You think you’re being smart? You’re being manipulated. The system wants you dependent. They don’t want you cured-they want you buying drops for life. I stopped my drops. My pressure didn’t go up. My vision didn’t get worse. Coincidence? Or proof that the whole thing is a scam?
And don’t even get me started on the "anxiety" people are talking about. Get a grip. Stop being emotional. You’re not dying. You’re just being told you might go blind. So what? Life’s a gamble. Stop paying for the ticket.
William Chin
December 12, 2025 AT 07:41While I appreciate the clinical depth of this post, I must emphasize that the ethical responsibility of the ophthalmological community extends beyond mere diagnostic precision and pharmacological intervention. The psychological burden imposed upon patients by the persistent ambiguity of disease progression-particularly in normal-tension glaucoma-constitutes a form of institutionalized medical anxiety. The current paradigm, which reduces complex neurodegenerative pathology to a single metric (IOP), is not only reductionist, but potentially harmful. We must, as practitioners and as a society, reorient our approach toward holistic, biopsychosocial models of care. The optic nerve is not a hydraulic system. It is a living, dynamic structure embedded within a neurovascular unit that responds to systemic, metabolic, and even emotional stressors. To treat it as anything less is to fail in our most fundamental duty: to heal, not merely to manage.
Furthermore, the commercialization of diagnostic technologies such as OCT and home tonometry, while ostensibly beneficial, has created a new class of medical consumers who equate surveillance with safety. This is not health. This is surveillance capitalism masquerading as preventive medicine.