What Exactly Is Lower GI Bleeding?
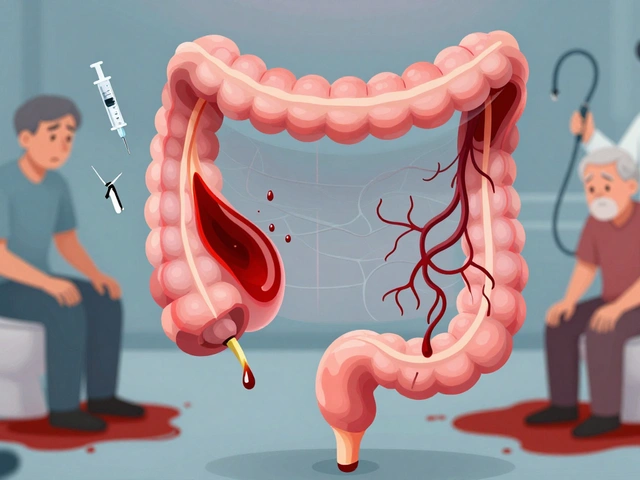
Lower gastrointestinal (GI) bleeding means blood is coming from somewhere in your colon, rectum, or anus - anything below the ligament of Treitz. You’ll usually notice it as bright red or maroon blood in your stool, sometimes in large amounts. It’s not always painful. In fact, the most common causes, like diverticula and angiodysplasia, often cause bleeding without any cramps or discomfort. This is why many people ignore it until they feel dizzy, weak, or see blood pooling in the toilet.
It’s more common in people over 60. About 20 to 27 out of every 100,000 adults experience it each year. While it sounds scary, most cases stop on their own. But knowing what’s causing it makes all the difference in treatment - and preventing it from coming back.
Diverticula: The #1 Cause of Sudden, Heavy Bleeding
Diverticula are small, balloon-like pouches that stick out from the wall of your colon. They’re super common - nearly half of people over 60 have them. Most never cause problems. But when one of these pouches develops a weak spot where a blood vessel runs close to the surface, that vessel can rupture. No inflammation. No infection. Just a sudden, painless gush of blood.
This is diverticular bleeding, and it’s responsible for 30% to 50% of all hospital admissions for lower GI bleeding. The blood comes out fast and heavy - sometimes enough to make you feel faint. You might see a whole cup of bright red blood in one go. It’s alarming, but the good news? About 80% of these bleeds stop by themselves within 24 hours.
What makes it tricky is that it looks just like other causes. That’s why doctors can’t just guess. You need tests. And even if the bleeding stops, you still need a colonoscopy to confirm it’s diverticula and not something more serious, like cancer.
Angiodysplasia: The Silent Bleeder That Drains You Slowly
Angiodysplasia - also called vascular ectasia or AVM - is a tangle of abnormal blood vessels in the colon wall. It’s most often found in the right side of the colon, especially in people over 70. Unlike diverticula, this isn’t a sudden explosion. It’s a slow drip.
People with angiodysplasia don’t usually notice bright red blood. Instead, they get tired. They feel weak. Their lips turn pale. They’re diagnosed with iron deficiency anemia after months of unnoticed blood loss. That’s because the bleeding is small, steady, and hidden. Over time, it chews through their iron stores. Many patients go to the doctor for fatigue and only find out they’ve been bleeding internally for over a year.
Here’s the twist: angiodysplasia is linked to heart problems too. If you have aortic stenosis - a narrowed heart valve - the force of blood rushing through it can break down a key clotting protein called von Willebrand factor. That makes you more likely to bleed from these fragile vessels. So if you’re over 70, have heart valve disease, and keep getting anemia, your doctor should check for angiodysplasia.
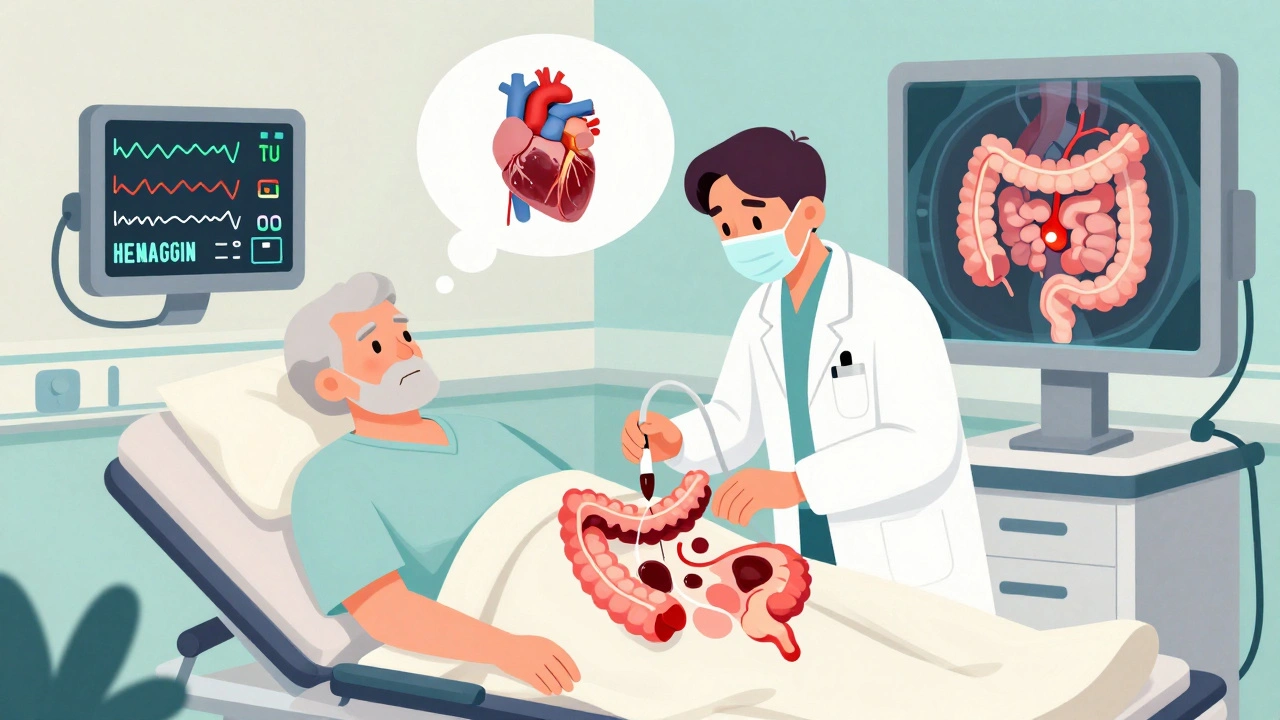
How Doctors Figure Out What’s Causing the Bleed
When you show up with GI bleeding, the first thing the team does is stabilize you. They check your blood pressure, heart rate, and hemoglobin. If your hemoglobin is below 10 g/dL, you’re losing blood fast. They’ll start IV fluids and may give you a blood transfusion.
Then comes the key test: colonoscopy. It’s the gold standard. Done within 24 hours of admission, it finds the source in over 80% of cases and can treat it at the same time. Even if you’re still bleeding, they’ll do it. They’ll use a mix of IV fluids and a drug called erythromycin to clear the bowel fast - no need to wait for a perfect prep.
But what if the colonoscopy shows nothing? That’s when things get harder. About 10% to 15% of bleeds come from the small intestine - a place colonoscopes can’t reach. That’s when doctors turn to other tools:
- CT angiography: This scan finds active bleeding if it’s happening at a rate faster than half a milliliter per minute. It’s fast, accurate (85% sensitivity), and great when you’re too unstable for endoscopy.
- Capsule endoscopy: You swallow a tiny camera. It takes thousands of pictures as it moves through your gut. It finds the cause in 62% of cases where colonoscopy was negative. But it’s not perfect - in 15% of cases, the capsule gets stuck if there’s a hidden narrowing.
- Device-assisted enteroscopy: This uses special scopes that can reach deep into the small bowel. It finds the problem in 71% of cases, but it’s complex and only available at big hospitals.
Treatment: What Happens After the Diagnosis?
For diverticular bleeding, if it stops on its own, you’re usually fine. Rest, fluids, and monitoring are enough. But if it keeps bleeding or comes back, endoscopic treatment is next. Doctors use epinephrine injections to shrink the vessel, then apply heat (thermal coagulation) to seal it. This works in 85% to 90% of cases. Still, about 1 in 5 people will bleed again within a year.
For angiodysplasia, the go-to treatment is argon plasma coagulation (APC). It’s like using a focused beam of ionized gas to burn the abnormal vessels. It stops the bleeding right away in 80% to 90% of cases. But the problem? It doesn’t fix the underlying issue. The vessels can regrow. Up to 40% of patients bleed again within two years.
That’s where new options come in. If you keep rebleeding, your doctor might try thalidomide - a drug usually used for cancer or leprosy. A 2019 study showed it cuts transfusion needs by 70% in people with recurrent angiodysplasia. Another option is octreotide, a hormone-like drug given as a daily injection. It helps reduce blood flow to the vessels.
Surgery is rare, but if one area of the colon keeps bleeding - like the cecum for angiodysplasia or a specific segment for diverticula - removing that part can be life-changing. Right hemicolectomy is the standard for stubborn right-sided angiodysplasia.
What You Need to Know About Recovery and Prevention
Most people recover well. The 30-day death rate for diverticular bleeding is 10% to 22%, but that’s mostly because patients are older and have other health problems - heart disease, kidney failure, diabetes - not because of the bleed itself. Angiodysplasia has a lower death rate (5% to 10%) but a much higher chance of returning.
There’s no surefire way to prevent diverticula from forming. But once you’ve had a bleed, avoiding NSAIDs (like ibuprofen or naproxen) is critical. These drugs increase bleeding risk. Also, make sure your iron levels are checked regularly, even if you’re not bleeding. Many people stay anemic because they don’t take supplements long enough.
For angiodysplasia, the focus is on catching it early. If you’re over 70 and have unexplained anemia, don’t wait. Ask for a colonoscopy. And if you have heart valve disease, mention it - it’s a major clue.
Technology is helping too. New AI tools built into colonoscopes are spotting tiny angiodysplasia lesions that human eyes miss - improving detection by 35%. And newer endoscopic clips are sealing diverticular bleeds with 92% success in recent trials.

What Happens If It Keeps Coming Back?
Recurrent bleeding is the real challenge. Patients often go through years of tests, false negatives, and frustration. One patient group reported an average of 18 months from first symptoms to diagnosis. Many had three or more negative colonoscopies before angiodysplasia was finally found.
If you’ve had two or more episodes of unexplained GI bleeding, you need a plan. That means working with a team - gastroenterologist, interventional radiologist, maybe even a surgeon. Don’t accept a “we couldn’t find anything” answer. Push for CT angiography or capsule endoscopy if colonoscopy was negative.
And remember: even if the bleeding stops, follow-up matters. Schedule regular blood tests. Keep track of your energy levels. If you start feeling tired again, it might not be aging - it might be another slow bleed.
When to Worry and When to Wait
Not every speck of blood means emergency. A few streaks on toilet paper after constipation? That’s likely hemorrhoids. But if you see:
- Large amounts of bright red blood
- Maroon-colored stool
- Dizziness, rapid heartbeat, or fainting
- Unexplained fatigue with pale skin
- then you need to get checked. Don’t wait. Don’t assume it’s ‘just hemorrhoids.’ The most dangerous causes - diverticula and angiodysplasia - often don’t hurt. They just bleed. And if you don’t know why, you can’t stop it.
What’s Next in Treatment?
Research is moving fast. A major NIH-funded trial (NCT04567891) is testing thalidomide versus placebo for recurrent angiodysplasia. Results are due in late 2024. If it works, it could become standard care.
Meanwhile, doctors are refining how they use existing tools. For example, combining capsule endoscopy with CT angiography improves diagnostic accuracy. And some hospitals now have dedicated GI bleeding protocols - teams that spring into action the moment a patient walks in.
Long-term, survival rates are good. Five-year survival for diverticular bleeding is 78%. For angiodysplasia, it’s 82%. But quality of life? That’s where the real battle is. Repeated hospital visits, transfusions, and the fear of another bleed take a toll.
Knowledge is power. Knowing the difference between diverticula and angiodysplasia isn’t just academic - it’s what guides your treatment, your follow-up, and your future.

Ella van Rij
December 1, 2025 AT 21:29Also, I swear I read somewhere that ‘orthography’ means ‘not typing like a drunk raccoon’ - but here we are, 2024, and my doctor still thinks ‘hemogoblin’ is a new energy drink.
ATUL BHARDWAJ
December 3, 2025 AT 08:56Steve World Shopping
December 4, 2025 AT 21:39Thalidomide’s anti-angiogenic properties via TNF-alpha suppression represent a paradigm shift - but only if you’re not contraindicated for teratogenicity or neuropathy. Which, statistically, most of your cohort is. So we’re back to square one.
Lynn Steiner
December 6, 2025 AT 19:00Why does no one tell you this can happen? I’m 52. I thought I was ‘just getting old.’ Turns out I was bleeding out. And no one warned me. #GutBetrayal
Alicia Marks
December 7, 2025 AT 02:54Paul Keller
December 8, 2025 AT 08:55Moreover, the reliance on erythromycin for bowel clearance, while expedient, lacks long-term safety data in elderly populations with QT prolongation risks. A more standardized protocol - perhaps incorporating motilin agonists with real-time hemodynamic monitoring - would elevate care beyond anecdotal efficacy.
Elizabeth Grace
December 8, 2025 AT 12:53My dad’s anemia was ‘just aging.’ Turns out it was his colon leaking. Slowly. For two years. I’m mad. And I’m telling everyone.
Steve Enck
December 10, 2025 AT 01:42This is not medicine. This is triage capitalism. The patient who survives diverticular bleeding is not a triumph of science - they are a statistical outlier who happened to bleed loudly enough to be heard. The silent bleeders? They become footnotes in discharge summaries.
Jay Everett
December 10, 2025 AT 09:17Colonoscopy? Done. APC? Done. Thalidomide? Trying it now. Honestly? Best advice I got: stop taking ibuprofen like it’s candy. And if you’re tired and pale? Don’t say ‘I’m just tired.’ Say ‘I think I’m bleeding inside.’
AI spotting lesions? YES. New clips? YES. But the real MVP? Asking for a second opinion. No one’s gonna fight for you like you will. 💪❤️
मनोज कुमार
December 12, 2025 AT 05:39