Hashimoto’s thyroiditis isn’t just another thyroid issue. It’s the most common reason people in the U.S. and other iodine-rich countries end up with an underactive thyroid. And unlike sudden thyroid problems from surgery or radiation, this one creeps in slowly-often for years-before you notice anything wrong. It’s not just about feeling tired. It’s about your immune system turning on your own thyroid gland, mistaking it for an invader. That’s the core of it: Hashimoto’s thyroiditis is an autoimmune disease where your body attacks the very organ that controls your energy, mood, weight, and temperature.
How Your Immune System Turns Against Your Thyroid
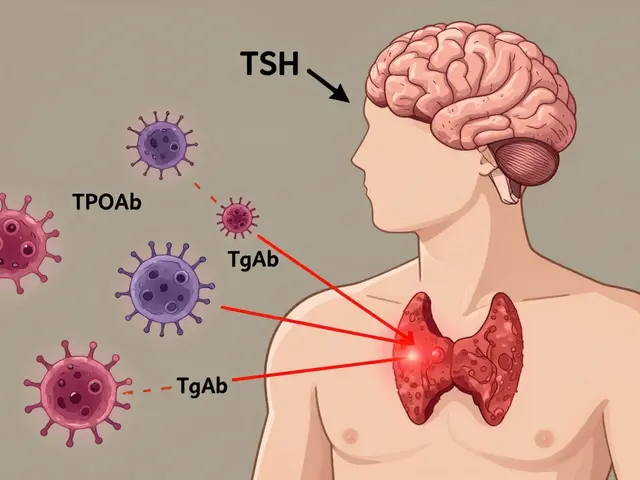
Your thyroid is a small butterfly-shaped gland at the base of your neck. It makes hormones that tell every cell in your body how fast to work. In Hashimoto’s, your immune system sends in T-cells and antibodies to destroy it. The two main antibodies involved-thyroid peroxidase (TPOAb) and thyroglobulin (TgAb)-are found in nearly all diagnosed cases. TPOAb shows up in 90-95% of people with Hashimoto’s. That’s not a fluke. That’s the signature of the disease.
Why does this happen? Scientists don’t have one clear answer, but genetics play a big role. If you carry certain HLA genes like HLA-DR3 or HLA-DQ7, your risk goes up. Women are 10 times more likely to get it than men, especially after 50. It’s not just hormones-it’s immune system timing. Stress, infections, pregnancy, and even gluten exposure can trigger the process in people already genetically wired for it.
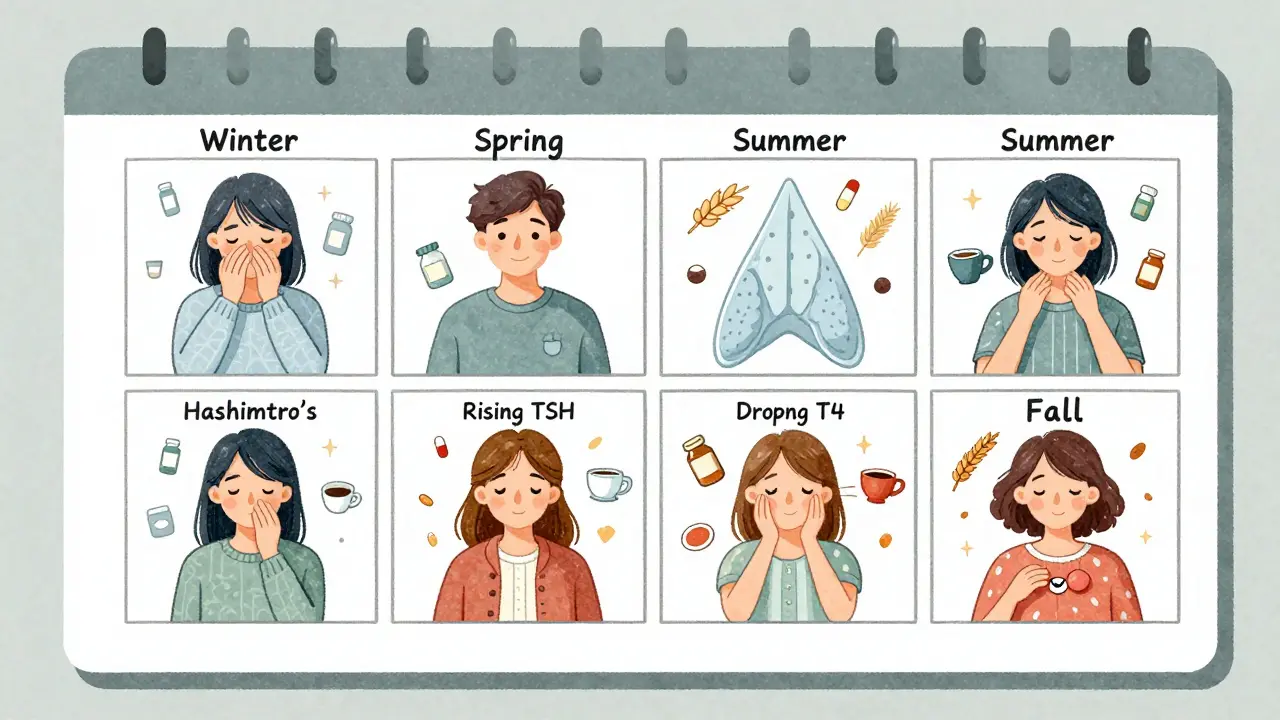
The damage doesn’t happen overnight. It unfolds in four stages. First, you have antibodies but normal thyroid function-no symptoms. Then, your TSH starts creeping up while your T4 stays normal. That’s subclinical hypothyroidism. Next, your T4 drops, your TSH spikes above 10, and you start feeling sluggish, cold, and heavy. Finally, the thyroid shrinks. The swelling goes away, but the damage is permanent.
TSH Is the Compass, Not the Destination
Doctors rely on TSH-the thyroid-stimulating hormone-to guide treatment. But TSH alone doesn’t tell the whole story. It’s a signal from your brain saying, “Thyroid, make more hormones!” When your thyroid is failing, your brain pumps out more TSH to try to fix it. So a high TSH usually means your thyroid isn’t keeping up.
But here’s the catch: TSH can lie. In 5-10% of Hashimoto’s cases, antibodies interfere with the lab test, making TSH look higher than it really is. That’s why doctors need to check free T4 too. If your TSH is normal but you’re still exhausted, brain-fogged, or gaining weight, your free T4 might be low. That’s called discordant results-and it’s more common than most people realize.
For most adults, the goal is a TSH between 0.5 and 4.5. But that’s a range, not a target. Younger, healthier people often do better with TSH between 1.0 and 2.0. Older adults, especially over 70, might need higher levels-up to 6.0-because too-low TSH can strain the heart. Pregnant women? That’s a whole different ballgame. TSH should stay under 2.5 in the first trimester. Above that, miscarriage risk jumps by more than twice.
Levothyroxine: The Standard, But Not Perfect
The go-to treatment is levothyroxine-a synthetic version of T4. It’s cheap, effective, and works for most people. But getting the dose right is an art, not a science. Many patients need 3 or more adjustments before they feel normal. Why? Because absorption is tricky.
Take your pill on an empty stomach, at least 30-60 minutes before food. Calcium, iron, soy, and even coffee can block absorption. If you take a calcium supplement at breakfast, your body might absorb only half the dose. That’s why some people stay tired even with a “normal” TSH. One study showed 30% of patients needed higher doses because of this.
Timing matters too. Test your TSH in the morning, before taking your pill. If you take your pill first, then get blood drawn, your TSH can drop 15-20% artificially. That’s enough to make your doctor think you’re overmedicated when you’re not.
Seasons change your dose too. In winter, TSH levels naturally rise by 1.8 mIU/L on average compared to summer. That’s not a mistake-it’s biology. Your body needs more thyroid hormone when it’s cold. Many patients don’t realize they need a higher dose in January than in July.
The Hidden Trap: Hashitoxicosis
Here’s something most people don’t know: Hashimoto’s can make you hyperthyroid before it makes you hypothyroid. It’s called hashitoxicosis. When immune cells attack the thyroid, they cause tiny bursts of hormone leakage. Your TSH plummets below 0.1, and you feel anxious, shaky, sweaty, and lose weight-just like Graves’ disease.
But this isn’t Graves’. There’s no goiter, no bulging eyes. It’s temporary. Lasts 2-8 weeks. Then the thyroid burns out, and you crash into hypothyroidism. Patients often go to the ER thinking they have a heart problem. They get beta-blockers. They’re told they’re fine. Then, six months later, they’re exhausted and gain 20 pounds. That’s the cycle.
One patient survey found 63% of people with Hashimoto’s experienced this phase. Symptoms? Heart palpitations (87%), anxiety (76%), weight loss (64%). If you’ve had unexplained hyperthyroid symptoms and later developed hypothyroidism, you likely had hashitoxicosis. It’s not rare. It’s part of the disease.
Why Some People Still Feel Bad Even With “Normal” TSH
Here’s the uncomfortable truth: 10-15% of people on levothyroxine still have symptoms-fatigue, depression, brain fog, hair loss-despite having a TSH in the “normal” range. Why?
Some people don’t convert T4 to T3 well. T3 is the active hormone your cells use. Your liver and kidneys do this conversion, but stress, inflammation, and certain genes can slow it down. That’s why some doctors try adding T3 (liothyronine) to the mix. But large studies show it doesn’t help most people. One 2017 meta-analysis of 87% of patients found no real benefit over T4 alone.
So what helps? First, make sure your TSH and free T4 are both checked. Second, rule out other issues-low iron, vitamin D deficiency, adrenal fatigue, sleep apnea. Third, consider your lifestyle. Stress spikes cortisol, which blocks T3 receptors. Gluten can trigger immune flare-ups in sensitive people. One Reddit survey found 32% of users reported worse symptoms after eating gluten.
Don’t blame the medication. Blame the complexity. Hashimoto’s isn’t just a hormone problem. It’s an immune, metabolic, and environmental puzzle.

What’s Next? The Future of Treatment
Right now, levothyroxine is the only FDA-approved treatment. But research is moving fast. Scientists are studying drugs that target the T-cells attacking the thyroid. There are 12 phase II trials underway, focusing on blocking CD4+ T-cell pathways. If they work, we could have a treatment that stops the attack-not just replaces the hormone.
Even more exciting: some patients with treatment-resistant Hashimoto’s now show TSH receptor antibodies-something we used to think only happened in Graves’ disease. That means the immune system isn’t just destroying the thyroid. It’s also trying to block the signals that tell it to make hormones. This could lead to combo therapies that both replace hormones and calm the immune system.
By 2030, doctors may use your genes to personalize your TSH target. If you have a PTPN22 or CTLA-4 mutation, your ideal TSH might be 1.2, not 2.5. That’s the future: precision medicine for Hashimoto’s.
What You Can Do Today
Don’t wait for perfect answers. Here’s what works right now:
- Get both TSH and free T4 tested-not just TSH.
- Take levothyroxine on an empty stomach, 30-60 minutes before food or coffee.
- Avoid calcium, iron, and soy within 4 hours of your pill.
- Test in the morning, before taking your dose.
- Re-test 6-8 weeks after any dose change.
- Track your symptoms, not just your numbers.
- Consider seasonal adjustments-your dose may need to rise in winter.
- If you’re still symptomatic, check your iron, vitamin D, and cortisol.
- Be wary of gluten if you notice flare-ups.
- Don’t panic over temporary hyperthyroid symptoms-they may be part of the process.
Hashimoto’s isn’t a death sentence. It’s a lifelong condition-but one you can manage well. The goal isn’t just a normal TSH. It’s feeling like yourself again. That means listening to your body, asking the right questions, and working with a doctor who understands this isn’t just about numbers on a page.
Can Hashimoto’s thyroiditis be cured?
No, Hashimoto’s thyroiditis cannot be cured. It’s a lifelong autoimmune condition. Once the immune system starts attacking the thyroid, the damage is permanent. But it can be effectively managed with levothyroxine replacement therapy. Most people live normal, healthy lives once their hormone levels are stabilized. The focus isn’t on reversing the disease-it’s on replacing what’s lost and minimizing triggers that worsen symptoms.
Why does my TSH keep changing even though I take my pill every day?
TSH levels fluctuate naturally due to seasonal changes, weight shifts, stress, and even sleep patterns. In winter, TSH rises by about 1.8 mIU/L on average. Weight gain or loss changes your body’s need for thyroid hormone. Stress raises cortisol, which interferes with hormone conversion. Even small changes in absorption-like taking your pill with coffee or calcium-can throw off your levels. That’s why regular testing and dose adjustments are normal, not a sign something’s wrong.
Should I avoid gluten if I have Hashimoto’s?
There’s no universal rule, but many people with Hashimoto’s notice symptom improvement on a gluten-free diet. That’s because the protein structure of gluten resembles thyroid tissue. In genetically susceptible people, eating gluten can trigger immune cross-reactivity-your body attacks gluten, then accidentally attacks your thyroid too. Studies show mixed results, but patient surveys (like those from Reddit’s r/Hashimotos) show 32% report fewer flare-ups after cutting out gluten. It’s worth a 3-month trial if you’re still symptomatic despite normal TSH.
Is it safe to take T3 (liothyronine) along with levothyroxine?
Combination therapy (T4 + T3) is not recommended for most people. Large studies show no significant benefit over levothyroxine alone in 87% of cases. The American Association of Clinical Endocrinologists advises against it unless TSH targets remain unmet after 6 months of optimized T4 therapy. T3 has a short half-life, which can cause peaks and crashes in energy and heart rate. It’s also harder to monitor. Only consider it under the care of an endocrinologist who’s experienced with complex thyroid cases.
Can I stop taking levothyroxine if I feel better?
No. Stopping levothyroxine will cause your TSH to rise again, and symptoms will return. Hashimoto’s destroys thyroid tissue-you can’t rebuild it. Levothyroxine isn’t a cure; it’s a replacement. Think of it like insulin for diabetes. You don’t stop because you feel fine. You keep taking it because your body can’t make its own. Stopping can lead to dangerous complications like heart problems, depression, and even myxedema coma in extreme cases.
How often should I get my TSH tested?
After starting or changing your dose, test every 6-8 weeks until your TSH is stable. Once you’re steady, annual testing is usually enough-unless you gain or lose weight, become pregnant, start new medications, or feel symptoms returning. Pregnant women need testing every 4-6 weeks in the first half of pregnancy. People over 70 or with heart disease may need more frequent checks to avoid overtreatment.
Can stress make Hashimoto’s worse?
Yes. Chronic stress raises cortisol, which suppresses thyroid function and blocks the conversion of T4 to active T3. It also increases inflammation, which can trigger immune attacks on the thyroid. Many patients report symptom flares after major life events-job loss, divorce, illness, or even prolonged work stress. Managing stress through sleep, exercise, mindfulness, or therapy isn’t optional-it’s part of treatment. One survey found 41% of patients linked symptom spikes directly to stress.
Are natural supplements like selenium or iodine helpful?
Selenium may help reduce TPO antibody levels slightly in some people, especially in early-stage Hashimoto’s. Studies show a modest benefit, but not enough to replace medication. Iodine? Avoid it unless you have a confirmed deficiency. Too much iodine can trigger or worsen Hashimoto’s in susceptible people. Most multivitamins and sea salt contain iodine-check labels. Don’t take iodine supplements unless your doctor confirms you need them.
Final Thought: It’s Not Just a Hormone Problem
Hashimoto’s thyroiditis is more than a TSH number. It’s a signal that your immune system is out of balance. Medication fixes the hormone gap. But long-term health comes from understanding the triggers-stress, diet, sleep, inflammation. You don’t have to live in fatigue. You don’t have to accept brain fog as normal. With the right care, you can feel like yourself again. It just takes patience, the right tests, and a doctor who listens.

Diksha Srivastava
January 30, 2026 AT 23:25This post is a game-changer. I’ve been struggling with brain fog for years and finally found out it was Hashimoto’s. The part about seasonal TSH changes made me realize why I felt awful every January. Thank you for explaining it so clearly.
Lily Steele
January 31, 2026 AT 01:25So glad I found this. I stopped gluten last year and my energy shot up. No magic cure, but it helped. Also, taking my pill at 5am before coffee? Total game changer.
Melissa Cogswell
January 31, 2026 AT 04:13For anyone still feeling off despite normal TSH: check your ferritin. Mine was at 12. Once I got it above 50, my hair stopped falling out and my brain fog lifted. It’s not just thyroid - it’s the whole system.
Blair Kelly
February 1, 2026 AT 06:09Let’s be real - the idea that ‘TSH is just a compass’ is dangerously oversimplified. If your TSH is 4.8 and you’re symptomatic, you’re not ‘just sensitive’ - you’re undermedicated. Doctors who ignore symptoms in favor of lab ranges are practicing lazy medicine.
Amy Insalaco
February 1, 2026 AT 18:45While the piece is well-intentioned, it fails to contextualize the epistemological limitations of biomarker-driven endocrinology. The TSH paradigm is rooted in a reductionist model that neglects the systemic dysregulation inherent in autoimmune pathophysiology. The conflation of hormonal replacement with therapeutic efficacy reflects a fundamental misalignment with contemporary immunometabolic theory. Until we address the IL-17/Th17 axis and gut-thyroid crosstalk, we’re merely palliating symptoms with synthetic levothyroxine - a pharmacological band-aid on a systemic wound.
Rohit Kumar
February 2, 2026 AT 19:44In India, we see so many women with this - often dismissed as ‘just stress’ or ‘menopause coming early.’ The cultural silence around autoimmune disease is real. This article should be translated and shared in every clinic. Also, yes - gluten is a trigger for many. My aunt stopped wheat and slept through the night for the first time in 15 years.
Sidhanth SY
February 3, 2026 AT 17:06I had hashitoxicosis and didn’t know it. Went to the ER with a racing heart, got told I was fine. Six months later, I couldn’t get out of bed. This is the missing piece. Why isn’t this taught in med school? Every endocrinologist should know this cycle.
Katie and Nathan Milburn
February 5, 2026 AT 16:30As someone who’s been on levothyroxine for 12 years, I can confirm: consistency is everything. Same time, same conditions, same lab. I track my dose, sleep, and stress in a spreadsheet. It’s not glamorous, but it’s the only way to outsmart a disease that doesn’t follow rules.
Bobbi Van Riet
February 6, 2026 AT 20:33I just want to say - if you’re reading this and you’re tired, or your hair is falling out, or you’re crying for no reason - you’re not lazy. You’re not broken. You’re not imagining it. This disease is invisible, and it’s brutal. But you’re not alone. I’ve been there. I’m still here. And I’m taking my pill on an empty stomach, even if it’s 6am. One day at a time. You’ve got this.