IPF Vaccines: What You Need to Know About Prevention and Research
When you hear IPF vaccines, vaccines designed to prevent or slow idiopathic pulmonary fibrosis, a progressive and often fatal lung disease. Also known as idiopathic pulmonary fibrosis prevention, it’s a concept still in early research—not yet a reality, but one that could change how we treat lung scarring forever. Right now, there’s no approved vaccine for IPF. But that doesn’t mean scientists aren’t working on it. Unlike flu or COVID-19, IPF isn’t caused by a virus you can target with a traditional shot. Instead, it’s a slow, unexplained scarring of the lungs, and researchers are now looking at ways to stop the immune system from attacking lung tissue—kind of like a vaccine that trains your body not to self-destruct.
What makes this tricky is that idiopathic pulmonary fibrosis, a chronic lung condition where lung tissue becomes thick and stiff, making breathing harder over time. Also known as pulmonary fibrosis, it’s often linked to aging, smoking, or environmental triggers. There’s no cure, and existing drugs only slow decline. That’s why the idea of a vaccine is so powerful. Imagine a treatment that doesn’t just manage symptoms but stops the disease before it takes hold. Studies are now exploring whether targeting specific proteins like TGF-beta or autoantibodies could act like a shield. Some early animal models show promise in reducing fibrosis by modulating immune responses—exactly what a vaccine would need to do.
And it’s not just about the lungs. pulmonary fibrosis research, the scientific effort to understand how lung scarring develops and how to stop it, including immune system involvement, genetic risks, and potential vaccine targets. Also known as lung fibrosis studies, it’s becoming a major focus in respiratory medicine. Scientists are connecting dots between chronic inflammation, viral infections like Epstein-Barr, and how they might trigger fibrosis in susceptible people. If a virus or repeated irritation kicks off the process, maybe a vaccine could block that trigger. Even if it doesn’t stop IPF completely, it might delay it by years—giving patients more time with better lung function.
Right now, the best defense against IPF is avoiding known risks: quitting smoking, using masks around dust or fumes, and managing GERD. But if you’re living with early signs—persistent dry cough, shortness of breath, unexplained fatigue—knowing that vaccine research is active gives hope. The next five years could bring breakthroughs. Clinical trials are starting to look at immune-modulating biologics that could evolve into preventive shots. This isn’t science fiction. It’s the next logical step after years of failed drug trials.
Below, you’ll find real-world guides on managing lung conditions, understanding medications that affect breathing, and spotting early signs of decline. While none of these are vaccines, they’re the tools you have now—and the context you need to understand why future breakthroughs matter.
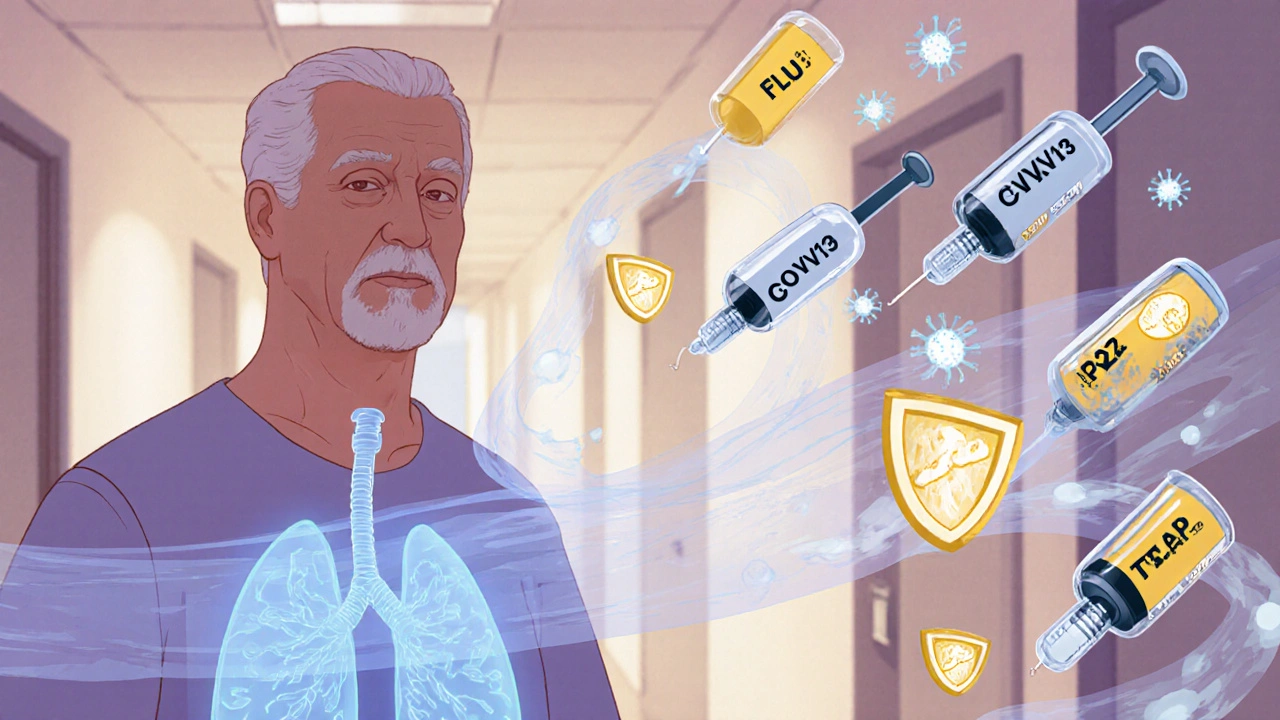
Why Vaccinations Are Critical for Idiopathic Pulmonary Fibrosis Patients
Vaccinations are a key defense for idiopathic pulmonary fibrosis patients, lowering infection risk and slowing disease progression. Learn which shots are essential, timing tips, safety facts, and practical steps to stay protected.
October 23 2025