Colon Bleeding: Causes, Signs, and What You Need to Know
When you see blood in your stool or on the toilet paper, it’s natural to panic. Colon bleeding, the presence of blood coming from the lower digestive tract, often from the colon or rectum. Also known as rectal bleeding, it’s not a disease itself—it’s a symptom, and it can mean anything from a harmless hemorrhoid to something that needs urgent care. The color matters. Bright red blood usually points to something closer to the anus, like hemorrhoids or anal fissures. Darker, maroon, or tarry stool suggests bleeding higher up in the colon or even the small intestine. Either way, it’s not something to ignore.
Gastrointestinal bleeding, a broader term that includes bleeding anywhere from the esophagus to the rectum is a category that colon bleeding falls under. It’s linked to conditions like diverticulosis, where small pouches in the colon wall burst; inflammatory bowel diseases like ulcerative colitis; or polyps that turn cancerous over time. Even infections or certain medications—like long-term NSAIDs—can irritate the lining and cause slow, steady bleeding. You might not feel pain, which makes it even more dangerous. Many people assume it’s just "old age" or "eating too much spicy food," but ignoring it can mean missing early signs of colon cancer.
Colon health, the overall condition of the large intestine, including its ability to process waste and maintain a protective barrier is tied directly to how often you see blood. Poor diet, lack of fiber, dehydration, and sedentary habits all weaken the colon’s natural defenses. That’s why so many of the posts here talk about gut health, medication safety, and digestive supplements. For example, if you’re taking blood thinners or NSAIDs regularly, you’re at higher risk. If you’re over 50 and haven’t had a colonoscopy, you’re flying blind. Colon bleeding isn’t just about what’s coming out—it’s about what’s going on inside.
What you’ll find below isn’t a list of scary stories. It’s a collection of real, practical posts that connect the dots between bleeding and the bigger picture: how medications interact with your gut, how supplements can help—or hurt—your digestive lining, how to track symptoms over time, and when to push for testing. You’ll see how things like drug interactions, when medications affect each other’s function in the body can silently damage your colon, how probiotics might help restore balance, and why tracking your meds with a simple log can catch problems before they become emergencies. This isn’t about fear. It’s about awareness. And the more you know, the better you can protect yourself.
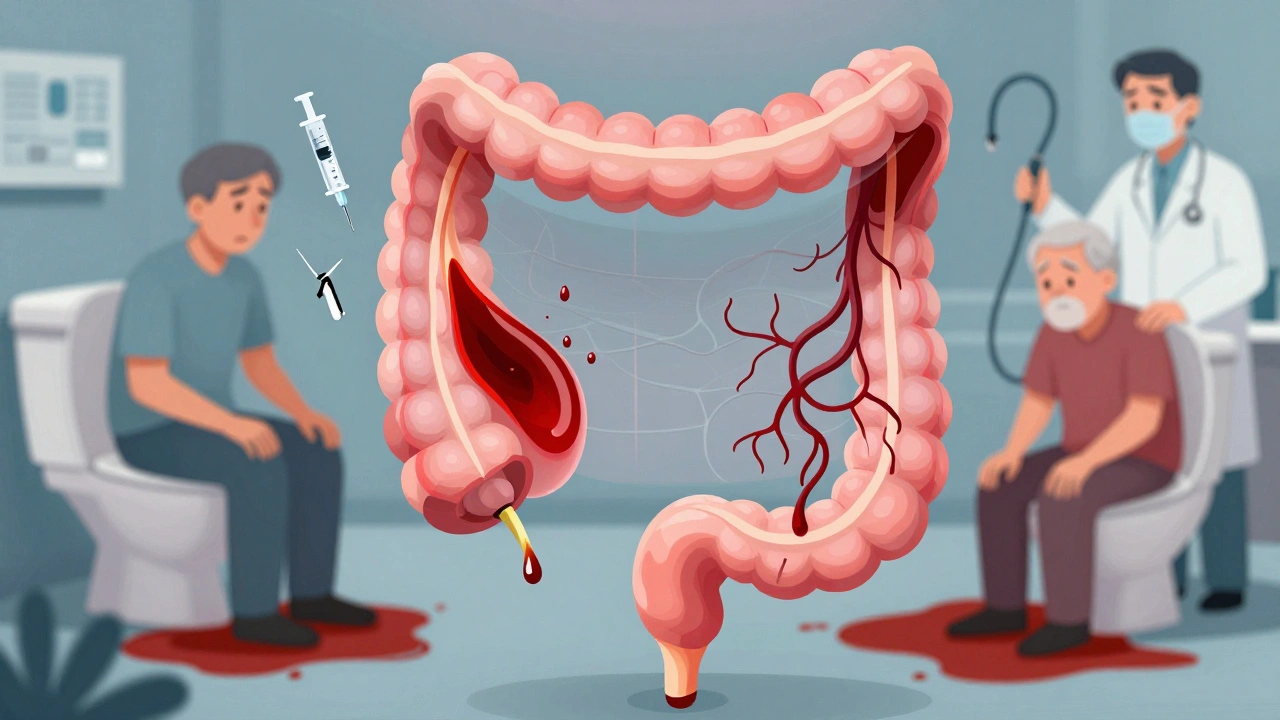
Lower GI Bleeding: Diverticula, Angiodysplasia, and How Doctors Diagnose It
Lower GI bleeding is often caused by diverticula or angiodysplasia, especially in older adults. Learn how doctors diagnose and treat these common but serious causes of rectal bleeding, and what to expect after diagnosis.
December 1 2025