Angiodysplasia: What It Is, How It's Diagnosed, and What You Can Do
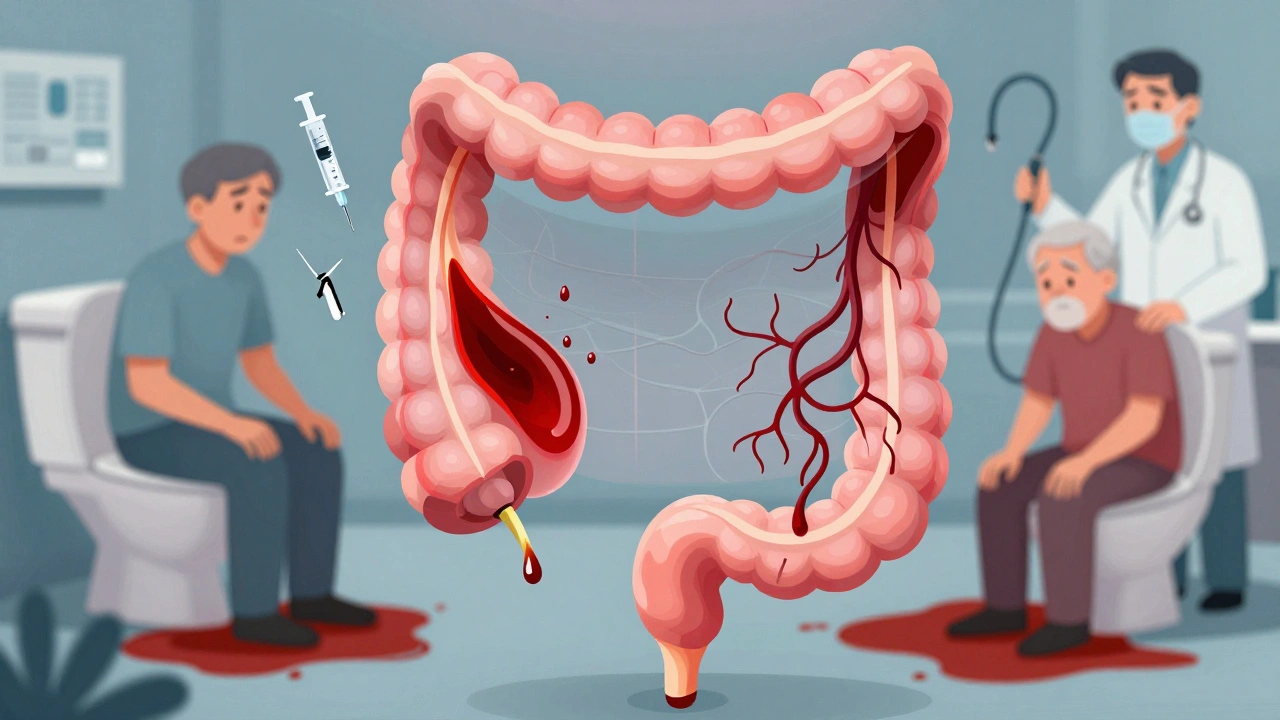
When you have unexplained bleeding in your gut and no polyps or ulcers show up, angiodysplasia, a type of abnormal blood vessel in the digestive tract that can bleed silently over time. Also known as arteriovenous malformation, it’s one of the most common reasons older adults end up with chronic anemia and need repeated blood transfusions. Unlike a bleeding ulcer, angiodysplasia doesn’t hurt. You won’t feel it until you’re weak, dizzy, or your stool turns dark—or your doctor notices your hemoglobin has been dropping for months.
This isn’t rare. It shows up in about 20% of people over 60 who have unexplained gastrointestinal bleeding. It’s most often found in the right side of the colon, near the cecum, where blood vessels are more fragile and prone to stretching under pressure. These vessels aren’t tumors. They’re just malformed, like a twisted garden hose that’s been left in the sun too long. Over time, the thin walls can rupture, causing slow, steady bleeding that drains your iron stores without warning. That’s why so many patients are diagnosed only after they’re already anemic—often with iron deficiency anemia, a condition caused by long-term blood loss that leaves you tired, pale, and short of breath. Many doctors miss it because standard colonoscopies don’t always catch these tiny, flat lesions unless they’re actively bleeding or the scope is carefully examined with high-definition imaging.
Diagnosis usually comes after ruling out other causes. If you’ve had negative tests for cancer, diverticulosis, or inflammatory bowel disease but still bleed, your doctor may order a capsule endoscopy, a swallowable camera that takes pictures as it moves through your intestines or a tagged red blood cell scan, a nuclear medicine test that pinpoints where bleeding is happening in real time. Sometimes, they’ll even do a repeat colonoscopy with special dye or use a technique called angiography to see the vessels directly. Treatment isn’t always needed—if the bleeding stops on its own, you might just need iron pills and regular blood checks. But if it keeps coming back, endoscopic therapy like cautery or argon plasma coagulation can seal off the vessels. In rare cases, surgery or embolization is required.
What you’ll find below are real, practical posts that cut through the noise. You’ll see how angiodysplasia connects to things like medication use, aging, and even how certain drugs can make bleeding worse. There’s no guesswork here—just clear facts on what works, what doesn’t, and what you need to ask your doctor next time you’re told your anemia has "no clear cause."
Lower GI Bleeding: Diverticula, Angiodysplasia, and How Doctors Diagnose It
Lower GI bleeding is often caused by diverticula or angiodysplasia, especially in older adults. Learn how doctors diagnose and treat these common but serious causes of rectal bleeding, and what to expect after diagnosis.
December 1 2025