Why phenytoin is different from other seizure meds
Phenytoin has been used since the 1930s to control seizures, and it still works - but it’s not like other epilepsy drugs. Even small changes in dose can cause big shifts in blood levels. That’s because phenytoin has non-linear pharmacokinetics. At low doses, your body clears it steadily. But as levels rise, the system gets overwhelmed. A 10% increase in dose might push levels up by 50%. That’s dangerous when the safe range is so tight: 10 to 20 mcg/mL.
And here’s the kicker: that range applies to total phenytoin in your blood. But only about 10% of it is actually active - the unbound fraction. The rest sticks to proteins like albumin. If your albumin drops - because you’re sick, malnourished, or have liver disease - your total phenytoin level might look fine, but your free (active) level could be way too high. That’s when you get toxicity: wobbly walking, blurred vision, confusion, even seizures.
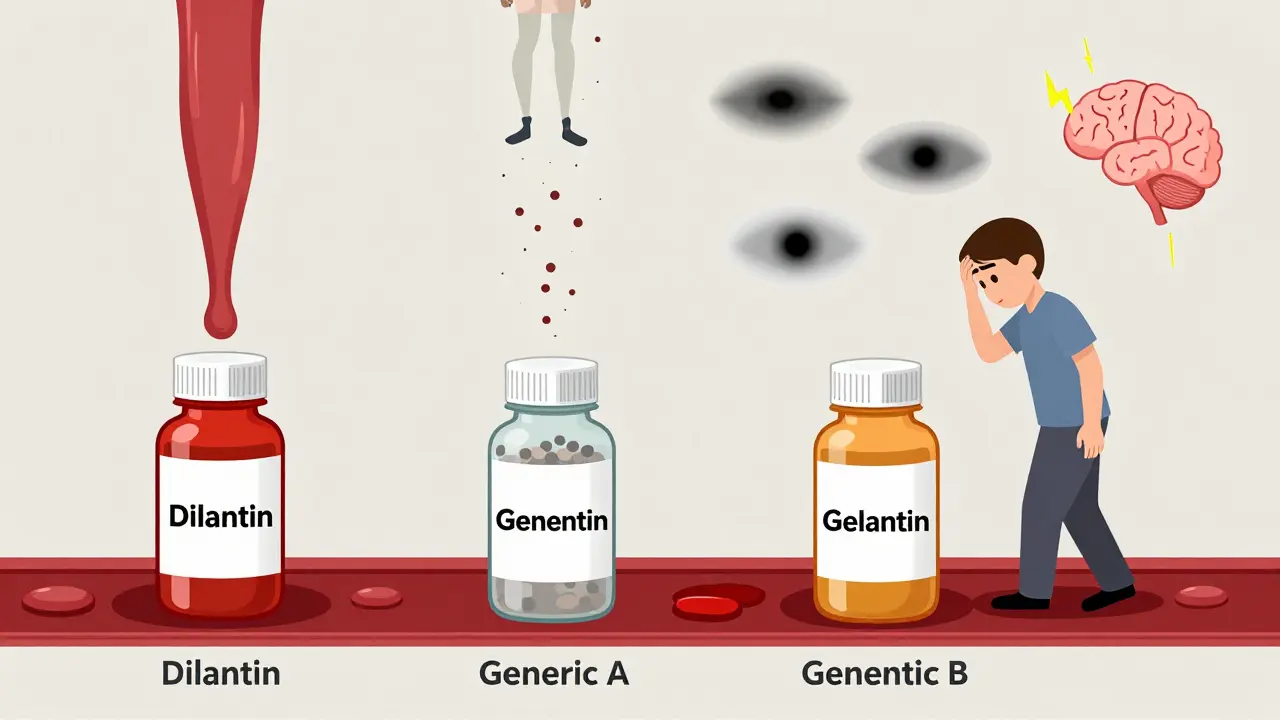
Generic phenytoin isn’t the same as brand-name
When you switch from Dilantin to a generic version, or from one generic to another, you’re not just changing the label. The FDA allows generics to vary by up to 20% in how much drug gets into your system compared to the original. That’s fine for most medicines. But for phenytoin? That’s a problem.
Imagine your level is at 15 mcg/mL - solidly in the middle of the safe zone. You switch to a generic that delivers 20% more drug. Your level could jump to 18 mcg/mL. Still okay? Maybe. But if you switch again - say, to a different generic that delivers 20% less - you could drop to 12 mcg/mL. That’s still in range, but what if your body actually needs 16 to stay seizure-free? Now you’re at risk of breakthrough seizures.
Studies show patients have more seizures or more side effects after switching phenytoin brands. It’s not always obvious. One person might feel fine. Another might get dizzy, nauseous, or start having tremors. No one knows why until the blood level is checked.
When you absolutely need a blood test
Don’t assume your doctor will automatically check your phenytoin level. Most people on long-term phenytoin don’t get routine monitoring. But there are times when it’s not optional:
- Right before switching from brand to generic - get a baseline level
- 5 to 10 days after switching - check again to make sure you’re still in range
- If you start feeling weird - dizziness, slurred speech, unsteady gait
- If you get sick, hospitalized, or start a new medicine
- If you’re pregnant, elderly, or have liver or kidney problems
Timing matters too. Don’t test right after a dose. Wait until just before your next pill - that’s the trough level. It tells you the lowest concentration in your system. For new doses or switches, wait at least 5 days before testing. Phenytoin takes time to build up. Testing too early gives false reassurance.
What your doctor should check besides phenytoin levels
Phenytoin doesn’t just affect your brain. It hits your bones, your liver, your blood, and even your gums. Long-term use can cause:
- Gingival hyperplasia - swollen, overgrown gums
- Vitamin D deficiency - leading to weak bones and fractures
- Folic acid deficiency - increasing risk of anemia and birth defects
- Low calcium and phosphate - affecting bone mineralization
- Hair growth in unwanted places, thickened facial features
That’s why before starting phenytoin, your doctor should check:
- Full blood count
- Liver function
- Albumin and electrolytes
- Vitamin D and calcium
- HLA-B*1502 gene test - if you’re of Han Chinese or Thai descent (this gene increases risk of severe skin reactions)
And you should get these repeated every 2 to 5 years, even if you feel fine. Bone health and blood counts don’t show symptoms until it’s too late.
How other drugs mess with phenytoin
Phenytoin doesn’t play well with others. It’s broken down by liver enzymes - and a lot of common drugs interfere with that process.
Some drugs slow down phenytoin breakdown, making levels rise dangerously:
- Amiodarone (heart medicine)
- Cimetidine (heartburn)
- Fluconazole (fungal infection)
- Metronidazole (antibiotic)
- Sodium valproate (another seizure drug)
Others speed up breakdown, making phenytoin less effective:
- Rifampin (tuberculosis treatment)
- Carbamazepine (another seizure drug)
- Alcohol (yes, even moderate drinking)
- Theophylline (asthma medicine)
When you switch phenytoin brands, your body might respond differently to these interactions. A drug that was fine before might now push your levels into the toxic range. That’s why it’s critical to tell your doctor about every medicine - even over-the-counter stuff or herbal supplements.

What to do if you’re low on albumin
If you’re sick, malnourished, or have liver disease, your albumin might be low. That changes everything. Your total phenytoin level could look normal - say, 14 mcg/mL - but your free level might be 25 mcg/mL. That’s toxic.
Here’s what your doctor should do:
- Check your albumin level
- If it’s below 30 g/L, ask for a free phenytoin test - not just total
- Don’t rely on correction formulas. They’re rough estimates
- Let your symptoms guide you. If you’re dizzy or unsteady, treat the patient, not the number
Some clinics routinely check free phenytoin in high-risk patients. Others don’t. If you’re in this group, ask. It’s not always covered by insurance, but it’s worth pushing for.
What the guidelines really say
The American Academy of Family Physicians says routine phenytoin monitoring doesn’t improve outcomes for everyone. That’s true. But they also say: monitor when switching formulations. The NHS in Scotland, the Specialist Pharmacy Service in the UK, and the American Epilepsy Society all agree: when you change phenytoin brands, test before and after.
It’s not about being paranoid. It’s about knowing that phenytoin is a precision tool. A slight change in formulation, a drop in albumin, a new antibiotic - any of these can tip you from safe to dangerous. And the consequences? Seizures, falls, confusion, coma, even death.
Bottom line: Don’t guess. Test.
If you’re on phenytoin - especially a generic - and you’ve switched brands recently, don’t wait for symptoms. Ask for a blood test. Make sure it’s a trough level, taken just before your next dose, at least 5 days after the switch.
If you’re elderly, have liver disease, are on other meds, or feel off - insist on a free phenytoin test. Don’t trust total levels alone.
And if you’re on phenytoin long-term, get your bone health checked every few years. Vitamin D, calcium, and folic acid matter. Your bones can’t wait.
Phenytoin saves lives. But it’s not a set-it-and-forget-it drug. It needs attention. And if you’re switching generics? That’s not a pharmacy decision - it’s a medical one. Talk to your doctor. Get tested. Stay safe.


Haley Graves
January 15, 2026 AT 11:18Diane Hendriks
January 15, 2026 AT 23:44Sohan Jindal
January 16, 2026 AT 07:47Frank Geurts
January 17, 2026 AT 18:58Annie Choi
January 18, 2026 AT 20:17Mike Berrange
January 20, 2026 AT 16:57Dan Mack
January 21, 2026 AT 00:32Amy Vickberg
January 21, 2026 AT 20:52Nishant Garg
January 22, 2026 AT 21:51Nicholas Urmaza
January 24, 2026 AT 14:57Sarah Mailloux
January 24, 2026 AT 18:55Nilesh Khedekar
January 26, 2026 AT 18:52Crystel Ann
January 27, 2026 AT 02:13Nat Young
January 28, 2026 AT 04:43