Snoring isn’t just annoying-it’s a sign your airway is collapsing while you sleep. If you’ve tried nasal strips, elevating your pillow, or sleeping on your side and still hear that loud, rhythmic noise, you’re not alone. Over 34 million American adults snore habitually, and nearly 40% of them are looking for a real solution. For many, oral appliance therapy with a mandibular advancement device (MAD) is the answer-not because it’s perfect, but because it actually works when nothing else does.
How a Mandibular Advancement Device Stops Snoring
Your snore happens when the muscles in your throat relax too much during sleep, causing your tongue and soft palate to fall back and partially block your airway. The result? Vibrating tissues = loud noise. A mandibular advancement device works by gently holding your lower jaw forward-just enough to keep that airway open. Think of it like pulling your chin slightly forward while you sleep, so your tongue doesn’t slide backward and choke your own breath. These devices aren’t fancy. Most look like a mouthguard, but they’re precision-engineered. Prescription MADs are made from semi-rigid acrylic with titanium connectors, molded to your exact teeth. Over-the-counter versions use thermoplastic that you soften in hot water and bite into. The key difference? Custom devices can be adjusted in tiny 0.5mm steps. That’s critical because the sweet spot for stopping snoring is usually between 8 and 10mm of forward movement from your natural bite. Research shows that when properly fitted, MADs reduce snoring intensity by 50-75%. One 2014 study found users saw a 63.2% drop in snoring frequency compared to placebo devices. That’s not magic-it’s physics. Move the jaw forward, open the airway, stop the vibration.Who Gets the Best Results?
Not everyone with snoring will benefit. MADs work best for people with mild to moderate obstructive sleep apnea-or those with primary snoring (no apnea, just noise). If you have severe sleep apnea, CPAP is still the gold standard. But if you can’t stand the mask, the noise, or the feeling of being tethered to a machine, MADs are your next best option. The ideal candidate has:- At least 6-8 healthy natural teeth in each jaw
- No serious TMJ disorder or jaw pain
- No advanced gum disease
- A body mass index (BMI) under 35
- No complete collapse of the soft tissues at the back of the throat (Mallampati Class I-III)
Custom vs. Over-the-Counter: The Real Difference
You’ll see ads for $99 snoring mouthpieces on Amazon. They’re tempting. But here’s the truth: custom MADs work twice as well. A 2015 meta-analysis found custom, titratable devices reduced snoring by 72.3%. Over-the-counter models? Only 48.6%. Why? Because they’re one-size-fits-none. Fixed advancement (usually 3-5mm) doesn’t match your anatomy. You might need 8mm. Or maybe only 5mm. A custom device lets your dentist fine-tune it over weeks. Top prescription brands like SomnoDent MAS and TAP 3 cost $1,800-$2,500. They’re durable, adjustable, and FDA-cleared as Class II medical devices. Over-the-counter options like Zyppah or Good Morning Snore Solution are cheaper, but they’re not adjustable, not custom, and rarely covered by insurance. If you’re serious about stopping snoring, don’t waste money on a $99 gadget. Get evaluated by a dental sleep specialist. The upfront cost is high, but the results? Life-changing for your partner-and your sleep quality.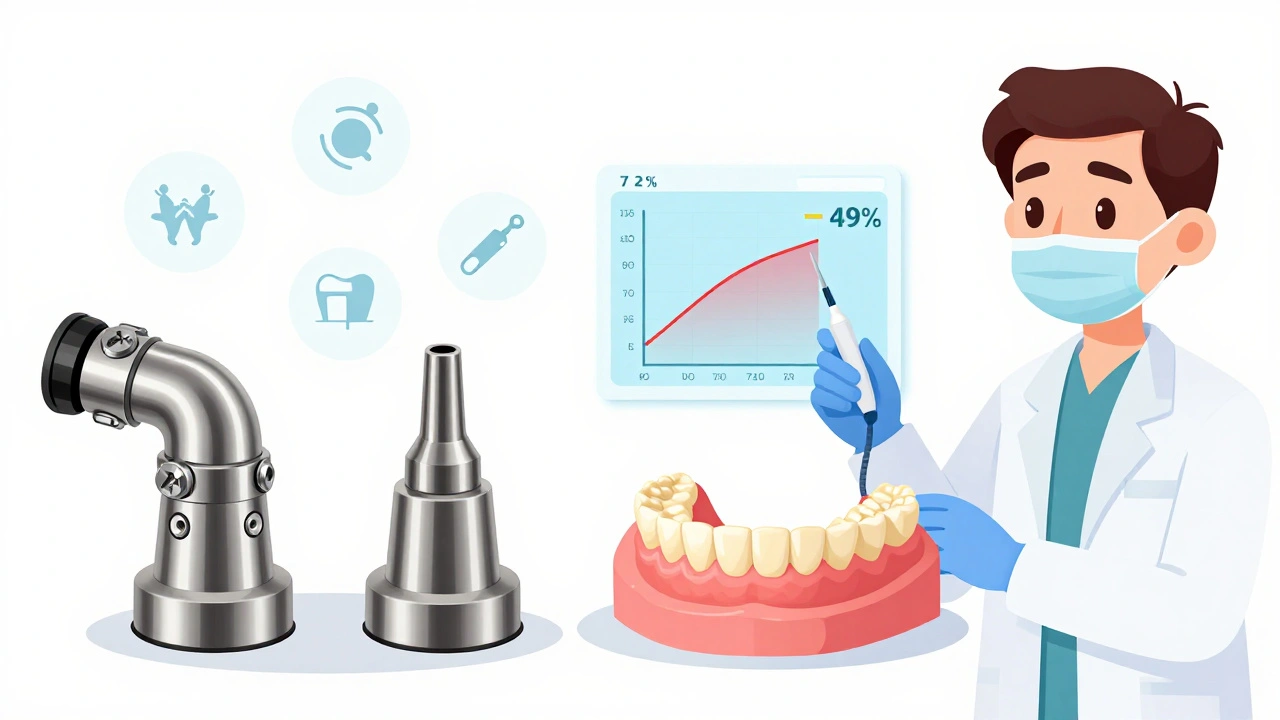
What to Expect When You Start Using One
Most people think they’ll slip the device in and wake up silent. It doesn’t work like that. The first week is rough. You’ll drool. Your jaw will ache. You might feel like you’re biting down on a golf ball. That’s normal. About 68% of users report morning jaw pain during the first few weeks. But here’s the trick: wear it for an hour or two during the day while you’re awake. That helps your muscles adjust. Most people find relief after 10-14 days. Titration-the process of slowly advancing the jaw-is the secret to success. Your dentist will likely start you at 2-3mm forward, then increase by 1mm every 3-5 days over 4-6 weeks. You’ll know you’ve hit the right setting when your partner says the snoring stopped, or your sleep tracker shows fewer breathing interruptions. Don’t rush it. Pushing too far too fast can cause lasting damage. That’s why professional fitting matters. DIY impressions? They’re 23% less accurate than in-office digital scans, according to a 2022 study. You want a perfect fit.The Hidden Costs: Dental Side Effects
MADs aren’t risk-free. The biggest concern? Your teeth and jaw change over time. About 25% of long-term users develop irreversible dental shifts. Your bite might feel off. Your front teeth could become loose. Your jaw joint might start clicking. In 14.7% of users who’ve worn MADs for 5+ years, orthodontic intervention was needed. That’s why regular dental check-ups every 6 months are non-negotiable. Your dentist needs to monitor your bite, your gum health, and your jaw joint. If you skip these visits, you’re gambling with your dental health. Other common side effects:- Excessive saliva (42.7% of users)
- Temporary tooth sensitivity (31%)
- Minor gum irritation

Why People Stick With It (And Why Others Quit)
CPAP has a 55% dropout rate after a year. MADs? Only 24% quit. Why? Because they’re quiet, portable, and don’t feel like medical equipment. One Reddit user, u/SnoringHusband, shared that his wife measured his snoring dropping from 65dB to 38dB-about the level of a quiet library. He called it “worth every penny.” That’s the kind of story you hear again and again. But here’s the flip side: 28.9% of users report persistent tooth discomfort. 14% need dental work after five years. And insurance? Only 38% of U.S. plans cover MADs. That means most people pay $2,000 out of pocket. For many, the trade-off is worth it. No hoses. No mask. No machine. Just a small device that fits in your pocket. You can travel with it. You can kiss your partner without embarrassment. You can sleep without waking yourself up every 10 minutes.What’s Next for Oral Appliance Therapy?
The field is evolving fast. In 2023, the FDA cleared the SomnoDent EVO 3-a device with built-in sensors that track your snoring and jaw position in real time, syncing data to a smartphone app. In 2024, a new AI-driven MAD from Sleep Solutions Inc. will automatically adjust your jaw position based on your breathing patterns. Researchers are even looking at genetic markers to predict who will respond best to MADs. In five years, your device might be custom-designed not just for your teeth-but for your DNA. But for now, the best tool is still the one your dentist fits you with. It’s not glamorous. It’s not cheap. But if you’re tired of sleepless nights and your partner’s side-eye, it’s the most effective non-surgical option out there.Is It Right for You? A Quick Checklist
Ask yourself these questions:- Have I had a sleep study to confirm I don’t have severe sleep apnea?
- Do I have at least 6-8 healthy teeth in each jaw?
- Do I have jaw pain or TMJ issues?
- Am I willing to pay $1,800-$2,500 (or find insurance coverage)?
- Am I okay with visiting a dentist every 6 months for check-ups?
- Do I want a solution that works without a mask, hose, or machine?
Can a mandibular advancement device cure sleep apnea?
MADs are effective for mild to moderate obstructive sleep apnea, reducing breathing interruptions by 50-70% in compliant users. But they’re not a cure. For severe sleep apnea, CPAP remains the most reliable treatment. Always get a sleep study before starting any therapy.
How long does it take to get used to a snoring mouthpiece?
Most people adapt within 10-14 days. Initial side effects like jaw soreness, drooling, or tooth pressure are common but usually fade. Wearing the device for 1-2 hours during the day can speed up adjustment. Full comfort often takes 3-4 weeks.
Do I need a prescription for a mandibular advancement device?
Over-the-counter MADs don’t require a prescription, but they’re far less effective. Custom devices are classified as Class II medical devices and require a prescription from a sleep specialist or dentist. Insurance coverage also requires a formal diagnosis and prescription.
Are there any long-term risks to using a MAD?
Yes. About 25% of long-term users develop permanent changes to their bite, tooth alignment, or jaw joint function. Regular dental check-ups every 6 months are essential to catch these early. Without monitoring, you risk needing braces, crowns, or TMJ treatment later.
Will my insurance cover a mandibular advancement device?
Only about 38% of U.S. commercial insurance plans cover MADs, and even then, you need a diagnosed sleep disorder and a prescription. Medicare rarely covers them unless you have moderate-to-severe OSA. Always check with your provider before investing in a custom device.


Shayne Smith
December 7, 2025 AT 02:21My husband started using one of those $99 Amazon gadgets last year. Snoring didn’t stop, but his saliva production went nuclear. We now have a whole drawer of damp pillows. Worth it? Absolutely not.
Ibrahim Yakubu
December 7, 2025 AT 19:58Y’all are missing the point. This isn’t about snoring-it’s about control. The jaw is the last bastion of autonomy you have in a world that wants you tethered to machines. MADs are rebellion wrapped in acrylic. They’re not medical devices, they’re symbols. You bite down, you assert your right to breathe without permission. The dentists don’t want you to know this. They profit off CPAP rentals. The system wants you dependent. Choose your jaw. Choose freedom.
Billy Schimmel
December 9, 2025 AT 19:51So you’re telling me I pay $2,000 to have my teeth slowly shift out of place, just so my wife can sleep through the night? And the insurance won’t cover it? Sounds like a scam designed by people who’ve never slept next to a snorer. I’ll just sleep on the couch. Again.
Karen Mitchell
December 10, 2025 AT 01:25It is deeply irresponsible to promote mandibular advancement devices as a viable alternative to CPAP without emphasizing the documented risk of irreversible dental malocclusion. The data is unequivocal: 25% long-term incidence of bite alteration. This is not a lifestyle product. It is a Class II medical device with significant biomechanical consequences. To recommend it casually is to endanger public health.
Geraldine Trainer-Cooper
December 11, 2025 AT 13:25Nava Jothy
December 13, 2025 AT 01:36Oh sweetie 🥺 you think a $2000 plastic mouthguard is the answer? Honey, your soul is snoring. You’re avoiding your trauma. You’re avoiding your grief. You’re avoiding the fact that you’ve been sleeping on your back since 2018 because you’re afraid of being vulnerable. The MAD is just a Band-Aid on a hemorrhage. Get therapy. Or at least a weighted blanket. 💔
olive ashley
December 13, 2025 AT 02:34Let me guess-this article was sponsored by SomnoDent. You know what they don’t tell you? That the same companies that sell these devices also own the sleep labs that diagnose you. They need you to be ‘mild to moderate’ so you keep buying their $2,000 toys. CPAP is cheaper in the long run. And the mask? You get used to it. The dental damage? That’s forever. Don’t fall for the quiet luxury scam.
Dan Cole
December 14, 2025 AT 04:48Let’s be clear: the only reason over-the-counter devices have 48.6% efficacy is because they’re designed by engineers who have never seen a human mandible. Custom MADs are not a luxury-they are a precision instrument. The 0.5mm adjustment capability is the difference between silence and a chainsaw. If you’re not working with a dental sleep specialist, you’re not treating snoring-you’re performing a crude biological experiment on yourself. The science is settled. The data is peer-reviewed. Stop wasting your money on Amazon gimmicks and invest in real medicine.
Andrew Frazier
December 15, 2025 AT 17:19USA got the best sleep tech in the world and some clown is buying plastic junk from India? I’ve seen these cheap mouthpieces-they’re made in factories where they don’t even wash their hands. You think your teeth are gonna thank you? Nah. You’re gonna end up in a dental chair crying because you trusted a 3-star review. Buy American. Or don’t sleep at all.