When your face suddenly turns red and feels hot-like you’ve just run a marathon in a sauna-it’s rarely just embarrassment. More often, it’s a medication you’re taking. Facial flushing from drugs is one of those side effects that catches people off guard. It’s not dangerous in most cases, but it’s embarrassing, uncomfortable, and sometimes enough to make someone stop taking a vital medicine altogether. If you’ve experienced this, you’re not alone. Thousands of people on common prescriptions deal with it every day.
What Causes Medication-Induced Facial Flushing?
Facial flushing happens when blood vessels in your face widen, letting more blood flow through. This isn’t just a skin-deep issue-it’s a direct effect of how certain drugs interact with your body’s nervous system and blood vessels. The redness usually hits your cheeks, nose, forehead, and sometimes your neck or chest. It can last minutes or hours, and it often comes with warmth, tingling, or even a slight burning sensation.
Some medications cause flushing because they’re designed to dilate blood vessels. Others trigger it as a side effect of how they work elsewhere in the body. For example, drugs that lower blood pressure or treat heart conditions often cause flushing because they relax the smooth muscle in arteries-including those in your face. It’s not a mistake. It’s built into how the drug works.
Common Medications That Trigger Flushing
Not all drugs cause flushing, but some are well-known culprits. Here are the most common ones:
- Vasodilators: These include nitroglycerin (a medication used to treat chest pain by widening blood vessels), hydralazine (a blood pressure drug), and minoxidil (used for severe hypertension). They’re meant to open up blood vessels, but they don’t discriminate-they open them everywhere, including your face.
- Calcium channel blockers: Drugs like amlodipine (a common blood pressure medication), nifedipine (used for angina), and diltiazem (a heart rhythm and blood pressure drug) are frequent offenders. Their job is to relax blood vessels, and your face pays the price.
- Niacin (vitamin B3): This one is famous. People take niacin to lower cholesterol, but the flush is so intense that many quit taking it. The reaction is caused by prostaglandins, chemicals that make blood vessels expand. Even taking aspirin beforehand only reduces the flush by about 30%.
- Opioids: Morphine (a strong painkiller) and similar drugs release histamine, which triggers redness and warmth. This isn’t an allergy-it’s a predictable chemical response.
- Vancomycin: This antibiotic can cause "red man syndrome" (a reaction characterized by flushing, rash, and sometimes low blood pressure). Slowing down the IV drip can prevent it.
- Sildenafil (Viagra): The same mechanism that helps with erectile dysfunction-widening blood vessels-can make your face glow. It’s common, harmless, and usually fades within an hour.
- Corticosteroids and immunosuppressants: Drugs like cyclosporine (used after organ transplants) and prednisone (a steroid for inflammation) can cause flushing by altering immune and vascular signals.
- Hormone therapies: Tamoxifen (for breast cancer), goserelin (for prostate cancer), and raloxifene (for osteoporosis) are all linked to flushing as part of their hormonal effects.
Why Some People Flush More Than Others
Not everyone on these drugs gets flushed. Genetics play a big role. People of East Asian descent often flush after drinking alcohol because they have a genetic variation that slows down alcohol breakdown. The same goes for some medications-your body’s ability to process them can make flushing more likely. Age, skin sensitivity, and even how fast you take the drug (like IV vs. pill) matter too.
Stress and heat can make it worse. If you’re already warm or anxious, flushing can spike. That’s why some people notice it more after a hot shower, during a meeting, or after eating spicy food.
How to Relieve Medication-Induced Flushing
There’s no one-size-fits-all fix, but several strategies help depending on the cause.
1. Talk to Your Doctor About Dose or Timing
If you’re on a drug like niacin or a calcium channel blocker, your doctor might lower the dose or switch you to a different medication. Sometimes, switching from an immediate-release pill to an extended-release version reduces flushing. For example, extended-release niacin causes less redness than regular niacin.
2. Take Aspirin or NSAIDs Beforehand
For niacin flush, taking 325 mg of aspirin 30 minutes before the dose can help. It doesn’t stop the flush completely, but it can cut it down by a third. Ibuprofen or indomethacin may work too. This won’t help for flushing caused by histamine (like with opioids) or other mechanisms, though.
3. Use Antihistamines for Histamine-Related Flushing
If your flushing comes with itching or feels like an allergic reaction (but isn’t), antihistamines like loratadine (a non-drowsy allergy pill) or cetirizine (another common antihistamine) may help. They’re most effective for opioid-induced flushing or reactions like red man syndrome.
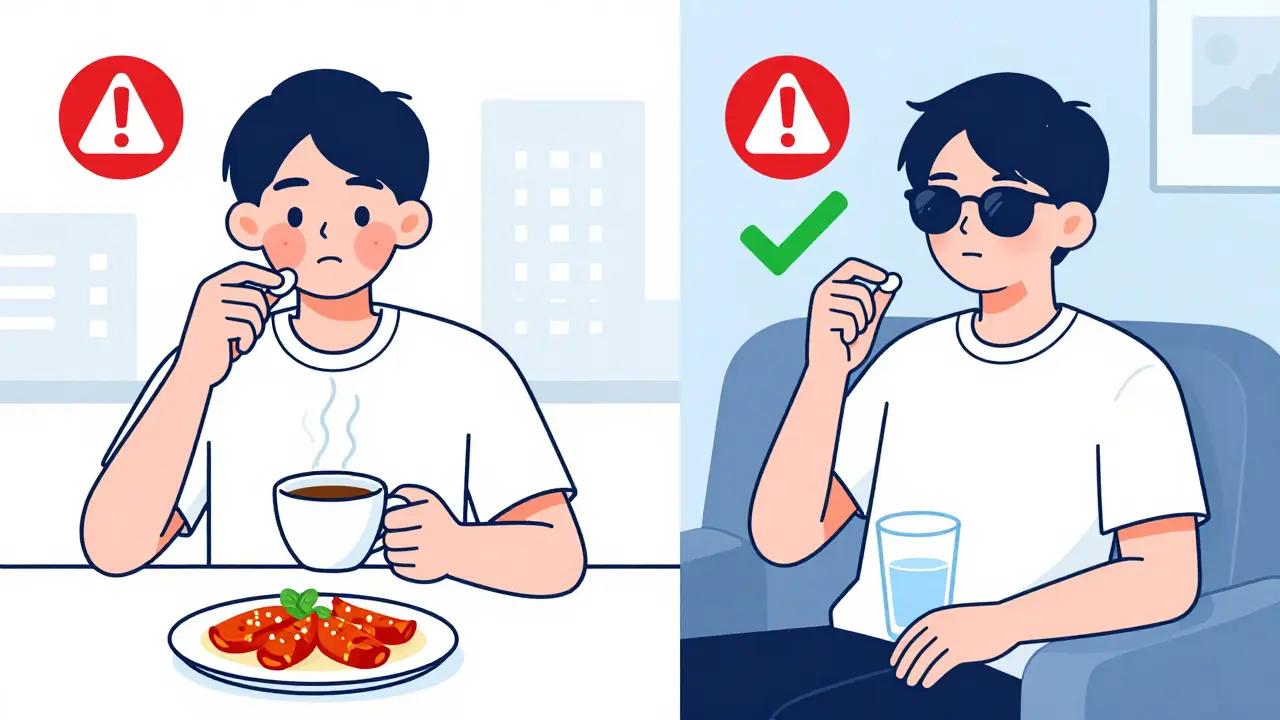
4. Avoid Triggers
Simple changes can make a big difference:
- Stay away from hot drinks, spicy food, and alcohol
- Avoid saunas, steam rooms, and intense heat
- Limit sun exposure-UV rays can make flushing worse
- Watch for MSG in food; it’s a known trigger for some
- Manage stress. Anxiety can trigger or worsen flushing
These aren’t just "tips." For many people, avoiding these triggers is the most effective way to reduce episodes.
5. Medications That Can Help Control Flushing
If lifestyle changes aren’t enough, doctors sometimes prescribe off-label drugs:
- Clonidine: This blood pressure medication also reduces nerve signals that cause flushing. It’s especially useful for people with chronic redness linked to anxiety or menopause.
- Beta-blockers: Drugs like propranolol (a heart medication) can calm the nervous system and reduce flushing triggered by stress or emotional spikes.
- Botulinum toxin (Botox): Injections into the face can temporarily block the nerves that cause flushing. Effects last 4-6 months. It’s not for everyone, but for severe cases where nothing else works, it’s an option.
- Laser therapy: Vascular lasers can target small, visible blood vessels in the face. It won’t stop flushing from medication, but it can reduce the permanent redness that builds up over time. Treatments are usually done in a dermatologist’s office.

When to Worry
Most flushing is harmless. But if it comes with:
- Difficulty breathing
- Dizziness or fainting
- Swelling of the lips, tongue, or throat
- Severe rash or hives
…then it could be an allergic reaction. Call your doctor or go to urgent care. True allergies are rare with flushing, but they can happen-especially with antibiotics or IV drugs.
What to Do Next
If you’re flushing and you’re not sure why:
- Write down when it happens-after taking a specific pill? After eating? When you’re stressed?
- Check your medication list. Look up each drug’s side effects.
- Don’t stop taking prescribed meds without talking to your doctor.
- Ask your doctor if switching drugs, adjusting the dose, or adding a blocker (like aspirin or an antihistamine) could help.
- Consider seeing a dermatologist if the redness lingers or becomes permanent.
Facial flushing from medications isn’t a sign you’re doing something wrong. It’s a side effect of modern medicine working the way it’s supposed to-just in places you didn’t expect. With the right adjustments, most people can manage it without giving up their treatment.
Can I stop my medication if it causes facial flushing?
No-not without talking to your doctor first. Many medications that cause flushing are essential for treating serious conditions like high blood pressure, heart disease, or cancer. Stopping them abruptly can be dangerous. Instead, ask your doctor about alternatives, dose adjustments, or ways to reduce the flush, like taking aspirin beforehand or switching to a slow-release form.
Is facial flushing from niacin normal?
Yes, it’s very common. About 90% of people who take immediate-release niacin experience flushing. It’s not dangerous, but it’s uncomfortable. Extended-release niacin causes less flushing, and taking aspirin 30 minutes before the dose can reduce it by up to 30%. Many people stick with it because the cholesterol-lowering benefits outweigh the temporary discomfort.
Does alcohol make medication flushing worse?
Yes, especially with certain drugs. Alcohol can intensify flushing from niacin, some antibiotics (like metronidazole), and even some blood pressure medications. It’s also a trigger on its own, particularly for people with a genetic variation that affects alcohol metabolism. If you flush easily, avoiding alcohol while on medication is a smart move.
Can stress cause facial flushing from medication?
Stress doesn’t cause the flushing itself, but it can make it much worse. When you’re anxious, your body releases adrenaline and other chemicals that widen blood vessels. If you’re already on a drug that causes flushing, stress can turn a mild redness into a full-blown episode. Managing stress through breathing techniques, therapy, or even beta-blockers can help reduce the severity.
Are there any long-term treatments for chronic facial flushing?
For persistent redness caused by repeated flushing, laser treatments can help reduce visible blood vessels. Botox injections can temporarily block the nerves that trigger flushing. These aren’t cures, but they offer relief when medications and lifestyle changes aren’t enough. Always discuss these options with a dermatologist or specialist familiar with medication side effects.


John Watts
February 11, 2026 AT 10:29Man, I wish I’d known all this before I started my niacin regimen. I thought I was dying the first time my face turned into a tomato. Turns out, it’s just biology being weird. Took me three months to figure out it wasn’t an allergic reaction-just my body saying, "Hey, vasodilation party!" Now I take aspirin 30 minutes before and it’s manageable. No more hiding in the bathroom after dinner.
Also, if you’re on this stuff, avoid spicy food like it’s a crime. Trust me, your face will thank you.
Tori Thenazi
February 11, 2026 AT 14:25Okay, but have you ever wondered if Big Pharma *wants* you to flush? I mean, think about it-niacin flush is so intense, people quit… then they go buy the "extended-release" version for 3x the price. And don’t get me started on Botox for flushing. That’s not medicine-that’s a money laundering scheme disguised as dermatology. They’re milking our embarrassment for profit.
Also, did you know the FDA approved vancomycin flushing as "normal"? That’s not normal-that’s negligence. Someone’s getting rich off our red faces.
Randy Harkins
February 13, 2026 AT 13:42This is such a helpful breakdown! I’ve been flushing since I started my blood pressure med, and I thought I was the only one. 😊 It’s reassuring to know it’s not dangerous-and even better, there are actual ways to manage it. I started taking low-dose aspirin before my pill and it cut the redness in half. Also, avoiding hot showers? Game changer. Thank you for writing this-I’m sharing it with my mom, who’s on the same meds.
Stay cool, everyone. Your face deserves a break. 🌿
Elan Ricarte
February 15, 2026 AT 05:10Let’s be real-this whole "flushing is harmless" narrative is a load of BS. I’ve had people stare at me like I’m a haunted carnival attraction. One guy asked if I was on drugs. I was on lisinopril. LISISOPRIL. Not crack. Not meth. Just a damn blood pressure pill.
And don’t even get me started on sildenafil. Yeah, it helps with erections, but it also turns your face into a stoplight. So congrats, pharma-you made a drug that helps men get hard and look like they just survived a heatwave. Brilliant marketing. Truly.
Also, why isn’t there a "flushing mode" on smartphones? Like, a filter that dims your redness before video calls? We’re living in 2024. Fix this.
Ritteka Goyal
February 15, 2026 AT 16:02As an Indian woman who’s been on tamoxifen for 4 years, I can tell you this flushing thing is NOT just about the drug-it’s about your entire body’s chemistry changing. I used to think I was just hot-natured, but nope. My mom said, "Beta, your hormones are screaming." And she’s right.
Here’s the thing no one tells you: stress + heat + Indian spices = full-blown Bollywood drama on your face. I’ve had people ask if I’m having a stroke. I had to carry a tiny fan in my purse. I even bought a cooling scarf. You think I’m joking? I’ve got receipts.
Also, if you’re from the West and think this is "just a side effect," you’ve never tried to walk into a Mumbai office with a glowing face. We don’t have AC everywhere. We fight. We adapt. We survive. And yes, I still take my pill. Because I’m not letting a red face stop me from living.
PS: Botox? I tried it. Felt like needles in my soul. Not worth it. Aspirin and chill-that’s my mantra.
Ashlyn Ellison
February 16, 2026 AT 01:49I just got my first flush after starting amlodipine. Took me 20 minutes to realize it wasn’t a fever. Now I just laugh. It’s like my face is doing yoga.
Alex Ogle
February 16, 2026 AT 14:47I’ve been on cyclosporine since my transplant. The flushing? Yeah. It’s constant. I used to avoid mirrors. Now? I just call it my "transplant glow."
What no one mentions is how it affects your social life. Dating? Forget it. Job interviews? I show up early so I can cool down. I’ve got a mini fan in my coat. I drink ice water like it’s my job.
And honestly? I don’t care anymore. This face? It’s survived chemo, rejection, and now… spontaneous sunburns without sun. It’s a badge. I wear it. Not proud. Just… resigned. And weirdly, kinda proud.
Patrick Jarillon
February 17, 2026 AT 13:37Everyone’s talking about aspirin and antihistamines like they’re magic potions. But have you considered that flushing might be your body’s way of saying, "This drug is poisoning you"? I mean, if your face turns red because a drug is forcing your blood vessels open-why are we treating it as a side effect instead of a warning?
What if the real solution isn’t aspirin or Botox… but stopping the damn drug? I’ve seen people flush from statins, beta-blockers, even SSRIs. And no one questions whether the drug is the problem or the solution.
Big Pharma doesn’t want you to stop. They want you to manage. And we’re all just… flushing along.
Also, did you know niacin was originally developed as a cheap liver treatment? Now it’s a billion-dollar supplement. Coincidence? I think not.
Monica Warnick
February 18, 2026 AT 22:23Okay, so I’ve been flushing for years… and I swear, it’s not the meds. It’s the Wi-Fi. Or maybe 5G. Or… the chemicals in the tap water. I live in a city with fluoridated water. And I take a beta-blocker. And I use a humidifier. And my face… glows. Like, it literally glows.
I’ve started wearing a silver foil hat under my hat. It helps. Slightly.
Also, I think the FDA is in on it. They know. They just don’t care. I’ve filed 12 complaints. No one responds. I’m starting a cult. We’ll call it "The Church of the Pale Face."
Anyone want to join? I have pamphlets. And a fan.
Jonah Mann
February 19, 2026 AT 23:47Just wanted to say-vancomycin red man syndrome? Yeah, that’s wild. I had it once during chemo. My whole upper body turned red, like I’d been boiled alive. Nurse said, "Slow the drip." I said, "You mean I’m not supposed to rush death?" She laughed. Then she gave me Benadryl. Saved my life.
Also, if you’re on opioids and flush? You’re not allergic. You’re just… biologically dramatic. My dog flushed once. I think he was on my pain meds. He looked like a cherry popsicle.
Angie Datuin
February 20, 2026 AT 09:18I’ve been on tamoxifen for 3 years. The flushing is rough, but honestly? The fact that I’m alive and my cancer hasn’t come back means more than a red face. I don’t use aspirin-I just wear loose shirts and drink cold water. And I’ve learned to smile when people ask if I’m hot.
It’s not glamorous. But it’s mine.
Frank Baumann
February 21, 2026 AT 14:04Let me tell you about the time I went to a job interview after taking my niacin. My face looked like a sunrise. The hiring manager asked if I was "in a sauna." I said, "No, just trying to lower my cholesterol." He nodded, then said, "We’ll call you."
They didn’t. I got the rejection email three days later. It said: "We found a candidate with a more… calm demeanor."
So now I take my pill at midnight. And I sleep with a fan. And I’ve started wearing a scarf to work. It’s not fashion. It’s survival.
Also, I’ve started a support group. We meet in the basement of a library. We call ourselves "The Flushed and Unashamed." We have cookies. And ice packs.
Camille Hall
February 22, 2026 AT 08:21For anyone struggling with flushing-don’t give up. You’re not alone. I’ve been on minoxidil for hair loss, and yes, my face glows like a lantern. But I also have more hair now than I did in college. So I’ll take the red cheeks. I’ve learned to laugh it off. And honestly? My coworkers think I’m just naturally radiant. I don’t correct them.
Small victories, right? You’ve got this. And if you need someone to vent to? I’m here. No judgment. Just solidarity. 💛