Reconstituted Suspensions: What They Are and Why Proper Use Matters
When a doctor prescribes a liquid medicine for a child or someone who can’t swallow pills, they often reach for a reconstituted suspension, a powdered medication mixed with water or another liquid to form a uniform liquid dose. Also known as oral suspension, it’s a practical solution for precise dosing, especially when exact amounts matter — like with antibiotics or seizure meds. But mixing it wrong can mean your medicine doesn’t work — or worse, makes you sick.
Reconstituted suspensions aren’t just watered-down pills. They’re carefully engineered formulas where the active drug is suspended in a thickening agent to keep particles evenly spread. If you add too much water, the dose becomes too weak. Too little, and it’s too thick to draw into a syringe. Some need to be shaken hard before every use — others don’t. The label tells you which. And shelf life? Many last only 14 days after mixing, even if the bottle says "use by 2026." That’s because once reconstituted, bacteria can grow, and the drug can break down. This isn’t theoretical — a 2020 study found nearly 1 in 5 caregivers mixed antibiotics incorrectly, leading to treatment failure.
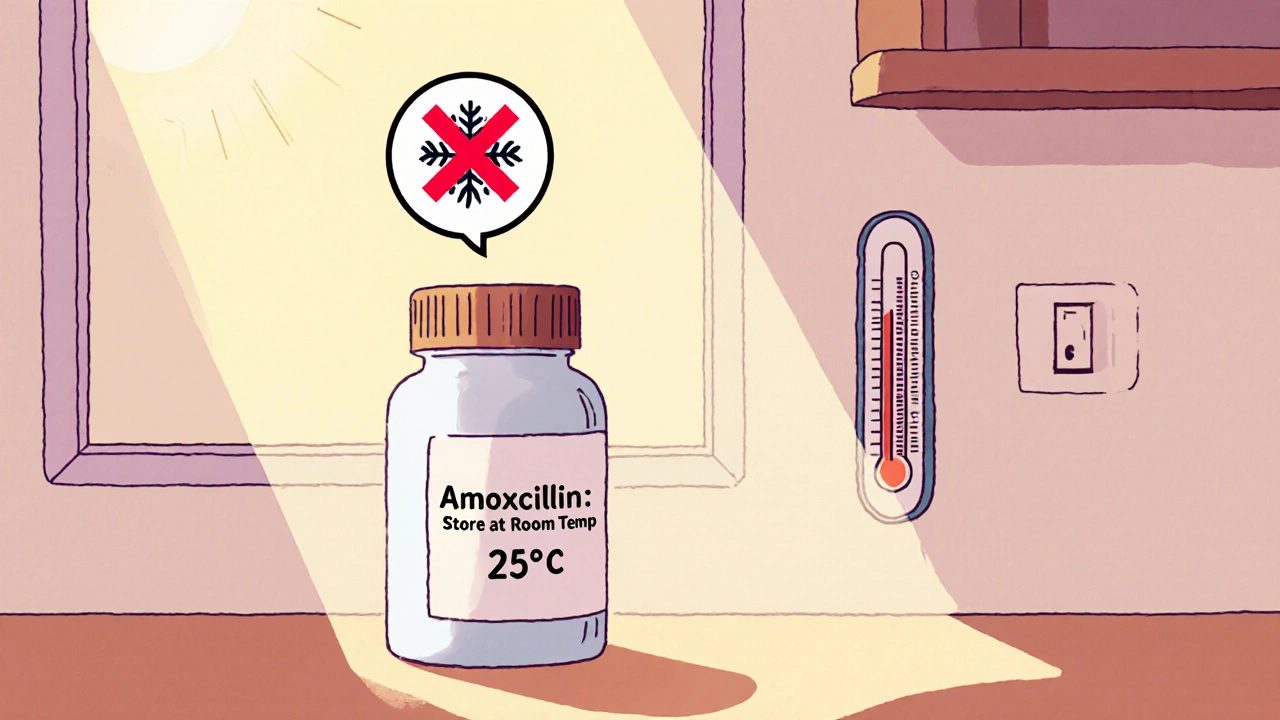
It’s not just about water. Some suspensions require specific liquids — never use juice or milk unless the pharmacist says so. Some need refrigeration after mixing. Others must stay at room temperature. The container matters too: you can’t just dump it into a random bottle. The original bottle is designed with the right seal, shape, and material to keep the suspension stable. And don’t forget the measuring tool. That plastic cup that came with the medicine? It’s often inaccurate. A proper oral syringe is safer, especially for kids.
These suspensions show up in common meds: amoxicillin for ear infections, cefdinir for pneumonia, azithromycin for strep throat. But they’re also used in chronic conditions — like antiretrovirals for HIV or seizure drugs for epilepsy. When a generic version is switched, the suspension formula might change slightly. That’s why tracking how you feel after a refill matters. If the medicine tastes different or doesn’t seem to work like before, it could be the suspension base, not the drug.
And then there’s the storage. A suspension left in a hot car or a sunny windowsill can separate, clump, or degrade. That’s why you’re told to keep it in the fridge — not because it’s "cold medicine," but because heat speeds up chemical breakdown. Even the way you shake it counts. A gentle swirl won’t do. You need a firm, full shake — 10 seconds or more — to re-suspend the particles. If you skip that, your child might get half the dose in the first sip and nothing in the last.
It’s easy to think, "It’s just liquid medicine," but reconstituted suspensions are one of the most error-prone parts of taking meds. A single mistake can mean a treatment fails, a infection spreads, or a seizure returns. That’s why pharmacists spend so much time explaining how to mix them — and why you should listen. You’re not just pouring powder into water. You’re preparing a medicine that needs to behave just right, every single time.
Below, you’ll find real-world guides on tracking medication changes, avoiding dangerous interactions, and using tools like medication logs to catch problems before they happen — all of which tie directly into getting reconstituted suspensions right.
How to Store Liquid Antibiotics and Reconstituted Suspensions Correctly
Learn how to properly store liquid antibiotics and reconstituted suspensions to ensure they remain effective. Discover temperature rules, shelf life, storage mistakes, and safe disposal methods.
November 20 2025