For years, parents were told to wait until their baby was two or three years old before introducing peanuts. The idea was simple: delay exposure, avoid allergy. But by 2015, the data told a different story. Peanut allergies in children had tripled since the 1990s. Emergency rooms were filling up. And the old advice? It wasn’t working.
Why the Old Advice Failed
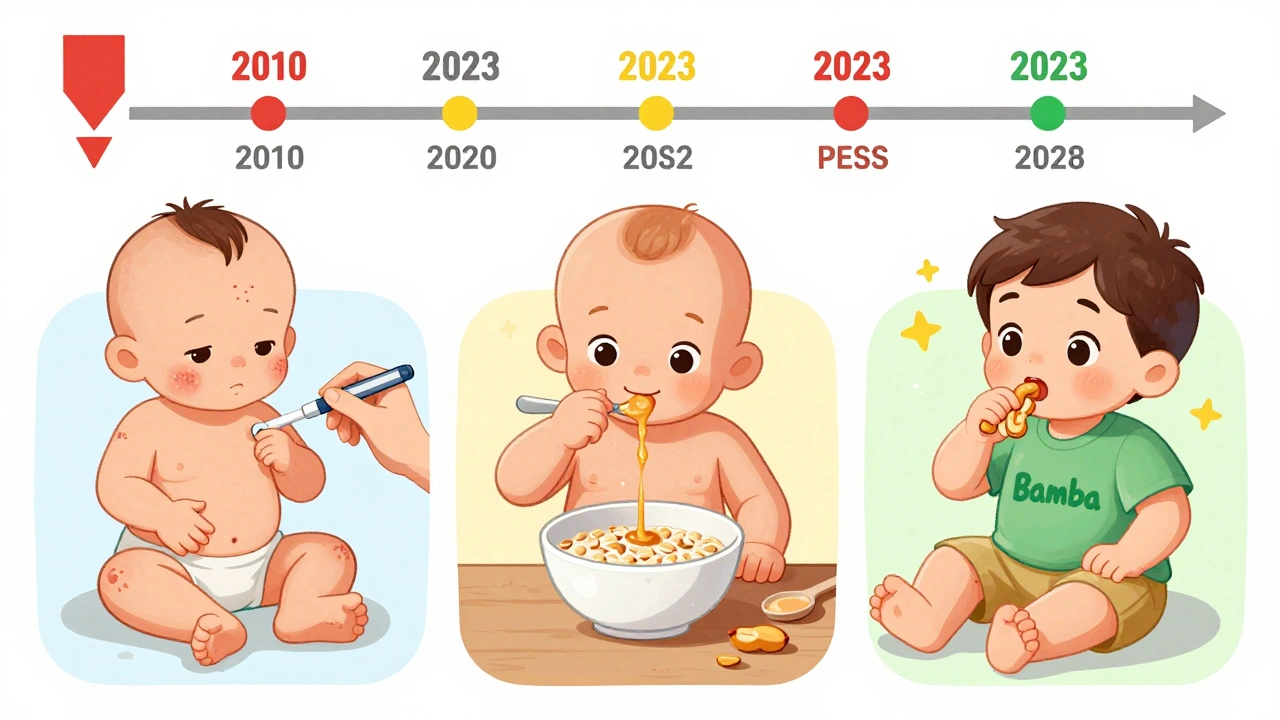
Before 2015, the American Academy of Pediatrics recommended delaying peanut exposure, especially for babies with eczema or egg allergies. That advice was based on fear, not science. And it backfired. Between 1997 and 2010, peanut allergies jumped from 0.4% to 2.0% in U.S. children. In Australia, rates rose too. Parents were doing everything right-waiting, avoiding, being cautious-and still, their kids were reacting. Then came the LEAP study. Led by Dr. Gideon Lack in London, it followed over 600 high-risk infants. Half were told to avoid peanuts entirely. The other half got peanut protein three times a week, starting between 4 and 11 months. By age 5, the group that ate peanuts had an 86% lower rate of peanut allergy. That wasn’t a small drop. It was a revolution.The New Guidelines: Three Risk Levels
In 2017, the National Institute of Allergy and Infectious Diseases (NIAID) released new guidelines based on LEAP and follow-up studies. They didn’t just say “introduce peanuts early.” They broke it down by risk.- High-risk infants (severe eczema, egg allergy): Introduce peanut between 4 and 6 months, after seeing a doctor. Testing might be done first-skin prick or blood test. If negative, start with 2 grams of peanut protein (about 2 teaspoons of smooth peanut butter mixed with water or formula), three times a week.
- Moderate-risk infants (mild to moderate eczema): Start around 6 months, at home. No testing needed. Just make sure it’s smooth peanut butter or a peanut-based puree, never whole peanuts.
- Low-risk infants (no eczema or food allergies): Introduce peanut anytime after starting solids, usually around 6 months. No special steps needed.
These aren’t suggestions. They’re evidence-backed rules. And they work.
What Counts as “Peanut Protein”?
Not all peanut products are safe-or even effective. Whole peanuts are a choking hazard. Peanut butter with added sugar or salt isn’t ideal. The studies used specific forms:- Smooth peanut butter mixed with warm water, breast milk, or formula (2 teaspoons = 2g peanut protein)
- Peanut flour or peanut powder stirred into infant cereal or pureed fruits
- Bamba (a puffed corn snack with peanut) - used in the LEAP study
For the first feeding, high-risk babies should be supervised by a doctor. For others, it’s fine to start at home. Watch for signs of reaction: hives, vomiting, swelling, trouble breathing. If any appear, stop and call your doctor.
Why Timing Matters
It’s not just about introducing peanuts. It’s about when. The window for prevention is narrow. Studies show the best results happen when peanut is introduced before 6 months. A 2023 analysis of LEAP and EAT studies found a 98% reduction in peanut allergy among babies who started early and stuck with it.Even small delays matter. Babies who started peanut after 10 months had five times higher allergy rates than those who started at 6 months, according to Australian research. And if you wait until age 2? You’ve missed the window. Early introduction doesn’t treat existing allergies-it prevents them.
Oral Immunotherapy (OIT) Is Not Prevention
Don’t confuse early introduction with oral immunotherapy (OIT). OIT is for kids who already have peanut allergy. It involves tiny, gradually increasing doses of peanut under medical supervision to build tolerance. It’s not a cure. It’s a management tool. And it carries risk-vomiting, anaphylaxis, even hospitalizations.Early introduction is different. It’s prevention. It’s giving a healthy baby peanut before the immune system has a chance to misfire. The goal isn’t to tolerate peanut. It’s to never develop the allergy at all.
Why So Few Parents Are Doing It
Despite the science, adoption is slow. A 2022 study found only 38.7% of high-risk infants in the U.S. received early peanut introduction. Why?- Parents are scared. They’ve been told for years that peanuts are dangerous.
- Doctors don’t always know the guidelines. One survey found only 54% of pediatricians could correctly describe them.
- There’s confusion about what’s safe. Some parents use crunchy peanut butter. Others give whole peanuts. Both are risky.
- Access is unequal. Black and Hispanic infants are 22% less likely to get early peanut exposure than white infants, according to a 2023 study.
It’s not just about knowledge. It’s about trust. Many parents want to do the right thing-but they need clear, calm guidance.
What Works in the Real World
In Australia, after updating their infant feeding guidelines in 2016, peanut allergy rates dropped sharply. The same pattern showed up in the U.S. After 2017, peanut allergy prevalence fell from 2.2% to 1.6% among children. That’s about 300,000 fewer kids with peanut allergy.What helped? Hospitals started handing out printed guides. Pediatricians began asking about peanut introduction at 4-month checkups. Some clinics offered peanut introduction clinics-where parents could bring their baby in for supervised first feeding.
Product makers noticed too. Peanut butter pouches designed for babies-smooth, no added sugar, pre-measured-grew 27% a year from 2018 to 2023. Companies like SpoonfulOne and Ready, Set, Food! now offer pre-measured allergen powders. They’re not magic. But they make it easier.

What Doesn’t Work
You’ve probably heard about probiotics, vitamin D, or eating peanuts while pregnant to prevent allergies. The science doesn’t back it up. Cochrane reviews found no clear benefit from any of these. The only proven method? Early introduction.And it’s not just peanuts. The EAT study showed that introducing multiple allergens-peanut, egg, milk, tree nuts-early and regularly reduced the risk of multiple food allergies. The same principle applies: early, consistent, safe exposure.
What Comes Next
Research is still evolving. The PRESTO trial, funded by NIAID with $35 million, is testing whether even earlier introduction-starting at 3 months-works better for the highest-risk babies. Results are expected in 2026.And long-term data from the LEAP study shows the protection lasts. Kids who ate peanut early and then avoided it for a year still didn’t develop allergies. That suggests true tolerance-not just temporary desensitization.
By 2030, if current trends continue and more parents follow the guidelines, peanut allergy rates could drop to 1.2%. That’s not just a number. It’s fewer ER visits. Fewer school bans. Fewer parents living in fear.
What You Can Do Today
If you’re expecting a baby or have one under 12 months:- Check for eczema or egg allergy. That tells you your baby’s risk level.
- Don’t wait. Start between 4 and 6 months, unless your doctor says otherwise.
- Use smooth peanut butter, peanut powder, or Bamba. Never whole peanuts.
- Give 2 grams of peanut protein (2 tsp peanut butter) three times a week.
- For high-risk babies, talk to your pediatrician first. They may refer you to an allergist.
- Watch for reactions. If you see hives, swelling, or vomiting, stop and call your doctor.
This isn’t about being perfect. It’s about being early. And consistent. One feeding won’t do it. But three times a week, for months? That’s how you change the odds.
Can I give my baby peanut butter straight from the jar?
No. Whole or chunky peanut butter is a choking hazard. Always mix smooth peanut butter with water, breast milk, or formula to make it thin and easy to swallow. You can also stir peanut powder into cereal or purees. Never give whole peanuts or peanut pieces to a baby under 4.
My baby has eczema. Should I test for peanut allergy before introducing it?
Yes, if your baby has severe eczema or an egg allergy. Talk to your pediatrician. They may refer you to an allergist for a skin prick or blood test. If the test is negative, you can start introducing peanut at home under supervision. If the test is positive, your allergist will guide you on safe introduction, possibly in a clinic setting.
Is it too late if my child is already 1 year old and hasn’t had peanut?
It’s not ideal, but it’s not too late. The strongest protection happens before 6 months, but introducing peanut between 1 and 5 years still reduces risk compared to never introducing it. Talk to your doctor first, especially if your child has eczema or other food allergies. They may recommend testing before home introduction.
Do I have to keep giving peanut forever?
Yes. Once you start, keep giving peanut regularly-at least three times a week. Stopping increases the chance of developing an allergy later. Studies show the protection lasts only if exposure continues. After age 5, if your child has tolerated peanut without reaction, you can reduce frequency, but don’t eliminate it entirely.
Can I introduce peanut if my family has a history of allergies?
Yes, and you should. Family history increases risk, but it doesn’t mean your baby will definitely develop an allergy. The guidelines don’t use family history alone to determine risk. Focus on eczema and egg allergy instead. If your baby has either, follow the high-risk protocol. If not, introduce peanut normally around 6 months.


Jordan Wall
December 3, 2025 AT 22:00Look, I get it - the LEAP study was peer-reviewed, blah blah. But have you seen the funding sources? NIAID? Big Pharma’s puppet show. 🤫 Peanut proteins are engineered to trigger immune responses - this is just another way to normalize allergens in infants before their gut flora even matures. The real agenda? More epinephrine auto-injectors sold. And don’t even get me started on Bamba - that’s a processed snack with palm oil and MSG. You’re not preventing allergies, you’re creating metabolic chaos. 🍿
Gareth Storer
December 5, 2025 AT 03:30Oh wow. So now we’re doing science by committee? Next they’ll tell us to feed babies asbestos to prevent lung cancer. Classic. ‘Avoidance backfired’ - yeah, because the parents were too stupid to read the fine print. Meanwhile, my kid’s allergic to air. Guess what? I didn’t introduce peanuts. I introduced common sense. 🤷♂️
Ashley Elliott
December 6, 2025 AT 07:58My daughter had severe eczema at 4 months. We did the skin test - negative. Started with 1 tsp peanut butter mixed into oatmeal, three times a week. No reaction. Now she’s 2, eats peanut butter straight off the spoon. No allergy. I’m just glad we listened to the guidelines instead of the internet. 🙏
Jessica Baydowicz
December 8, 2025 AT 05:12Y’all, this is the kind of info that changes LIVES. 🌟 I used to panic every time my toddler touched a peanut butter cracker. Now? We keep a jar in the pantry. No fear. No stress. Just peace. If you’re on the fence - just start small. A sprinkle of peanut powder in applesauce. You’ve got this. 💪
Augusta Barlow
December 9, 2025 AT 16:10Let’s be real - the entire peanut introduction craze is just corporate fear-mongering wrapped in science-speak. The real cause of the allergy surge? Glyphosate in the soil, GMO peanuts, and vaccines with aluminum adjuvants. The LEAP study? Funded by a company that sells peanut powder supplements. They want you hooked on their $30/month ‘allergen starter packs.’ Wake up. The FDA is in bed with Big Snack. My cousin’s kid developed anaphylaxis after ‘safe’ peanut exposure. Coincidence? I think not. And don’t get me started on how they’re pushing this in schools while banning crayons for being ‘toxic.’ The system is rigged. 🕵️♀️
Meanwhile, in the 1970s, kids ate peanut butter sandwiches daily. No allergies. No doctors. No tests. Just lunch. Now we’ve got pediatricians doing skin pricks like it’s a blood test for alien DNA. It’s not prevention - it’s normalization of medicalization. We’re turning parenting into a compliance checklist. And guess who profits? The ones selling the tests, the powders, the pouches. I’m not feeding my baby anything that comes in a branded pouch. Period.
My neighbor’s baby had a reaction after 2 grams of peanut butter. She didn’t even know she was supposed to wait until 6 months. The pediatrician blamed her. But the real problem? No one told her the truth - that the guidelines are still being tested. The 98% reduction? It’s from a subset of high-risk kids in controlled settings. Real-world parents? They’re winging it with Bamba and anxiety. And now we’re shaming the ones who wait. That’s not science. That’s social pressure with a white coat.
And what about the kids who are allergic despite early exposure? Are they just ‘bad luck’? Or is the science incomplete? Why isn’t anyone asking why 14% of high-risk kids still developed allergies? Why isn’t there a study on gut microbiome diversity before introduction? No - we just shove peanut butter down their throats and call it progress. I’d rather trust my grandma’s advice: ‘Wait till they’re walking.’
Also - why is this only about peanuts? Why not peanuts, eggs, milk, wheat, soy, fish? Are we just cherry-picking the one that makes the most money? And why is the ‘three times a week’ rule so rigid? What if my baby hates it? Do I force it? Is that trauma? Are we creating food anxiety before they can even talk? I’m not a lab rat. My child isn’t either.
And the racial disparity? Of course. Black and Hispanic families don’t have access to allergists, or the time off work to sit through supervised feedings. But instead of fixing that - we just blame them for not following guidelines they can’t afford. That’s not equity. That’s exploitation with a flowchart.
I’m not anti-science. I’m anti-corporate manipulation disguised as public health. If you want to give your baby peanut butter - fine. But don’t pretend this is a miracle. It’s a gamble with a fancy name.
Shofner Lehto
December 11, 2025 AT 08:48My son had moderate eczema. We introduced peanut butter at 6 months - mixed with applesauce. No issues. Now he’s 3 and loves PB&J. I’m not a doctor, but I followed the NIAID guidelines exactly. No testing, no panic. Just consistency. It worked. If you’re scared, start with 1/4 tsp. Build up slowly. You’re not rushing anything - you’re giving your child a gift of safety.
Rudy Van den Boogaert
December 12, 2025 AT 03:44I’m a dad of two. First kid? We waited till 3. Got the allergy. Second? We started at 5 months with smooth PB mixed into yogurt. Zero issues. I know it’s scary - I was terrified too. But the data is solid. This isn’t a gamble. It’s the opposite. Waiting is the risk. I wish I’d known this sooner.
John Filby
December 12, 2025 AT 19:17My sister’s baby had a reaction after 1 tsp of peanut butter. She freaked out, called 911 - turns out it was just a rash from the formula. But now she’s terrified to try again. I told her to wait a week and try again with 1/4 tsp. She did. No reaction. Now her kid eats peanut butter like it’s candy. 🤗 Don’t let one scare story stop you. Start small. Stay calm. You’ve got this.
Alex Piddington
December 13, 2025 AT 00:15Thank you for this comprehensive and evidence-based overview. The transition from avoidance to early introduction represents one of the most significant shifts in pediatric allergology in the past century. It is imperative that healthcare providers, educators, and caregivers alike be equipped with accurate, accessible information to ensure equitable implementation. The disparities in access - particularly among marginalized communities - must be addressed through systemic support, not individual blame. Continued research, such as the PRESTO trial, will further refine our understanding. For now, the data is clear: early, consistent exposure saves lives.
Libby Rees
December 14, 2025 AT 15:51My son is 7 months old. We introduced peanut butter at 6 months. Smooth, mixed with breast milk. No reaction. We’ve done it three times a week since. I read the guidelines. I talked to the pediatrician. I didn’t panic. It worked. Simple. Effective. No gimmicks. Just science.
Yasmine Hajar
December 16, 2025 AT 03:59OMG I just found this post and I’m crying. My daughter had a reaction at 10 months - we thought we were being careful by waiting. Turns out we waited TOO long. We didn’t know about the 4-6 month window. I feel so guilty. But now I’m telling everyone I know - don’t wait. If you have eczema? Go see the allergist. Don’t wait for your 6-month checkup - schedule it early. I’m so thankful for this info. I wish I’d known sooner. ❤️
Emmanuel Peter
December 18, 2025 AT 02:46Let’s be honest - this whole thing is a scam. The ‘86% reduction’? That’s from a tiny group of high-risk kids in the UK. Most parents don’t have access to allergists. Most babies aren’t even tested. So what’s the real success rate? 20%? 30%? And now we’re selling peanut powder for $25 a jar? That’s not prevention - that’s capitalism with a baby blanket. The real solution? Stop feeding kids processed food. Let them eat real food. Like, you know - actual peanuts. Not ‘peanut protein’ in a pouch. But no, that’s too old-school. We need a product. A brand. A subscription. 🤡