When you have asthma, your airways are inflamed - even when you feel fine. That hidden swelling is what makes you wheeze, cough, or struggle to breathe during flare-ups. But how do doctors know how bad that inflammation really is? Traditional tests like spirometry measure how well you can push air out of your lungs, but they don’t tell you why your lungs are struggling. That’s where FeNO testing comes in.
What Is FeNO Testing?
FeNO stands for Fractional Exhaled Nitric Oxide. It’s a simple, non-invasive test that measures how much nitric oxide is in your breath. Nitric oxide is a gas your body produces naturally, especially when there’s inflammation in your airways. In people with asthma, particularly those with allergic or eosinophilic asthma, this gas builds up as a direct sign of inflammation.
The test takes less than a minute. You breathe in deeply through a filter that removes outside air, then exhale slowly and steadily into a handheld device - like blowing out a candle, but slower and controlled. The machine reads the nitric oxide level in parts per billion (ppb). No needles. No blood draw. No discomfort. Even kids over five can do it.
Why FeNO Matters in Asthma Care
Most asthma treatments - especially inhaled corticosteroids - work by reducing airway inflammation. But not all asthma is the same. Some people have inflammation driven by allergies or immune cells called eosinophils. Others have inflammation from other causes, like pollution or infections. FeNO helps doctors spot the type that responds best to steroids.
Here’s what the numbers mean for adults:
- Below 25 ppb: Low inflammation - likely not driven by eosinophils
- 25-50 ppb: Moderate inflammation - steroid treatment may help
- Above 50 ppb: High inflammation - strong sign of active, steroid-responsive asthma
For children aged 5-12, the cutoff is 20 ppb. If your FeNO level is high, it doesn’t just confirm asthma - it tells your doctor your current treatment might not be working well enough. Studies show that adjusting medication based on FeNO levels can cut asthma flare-ups by up to 50%.
How FeNO Compares to Other Tests
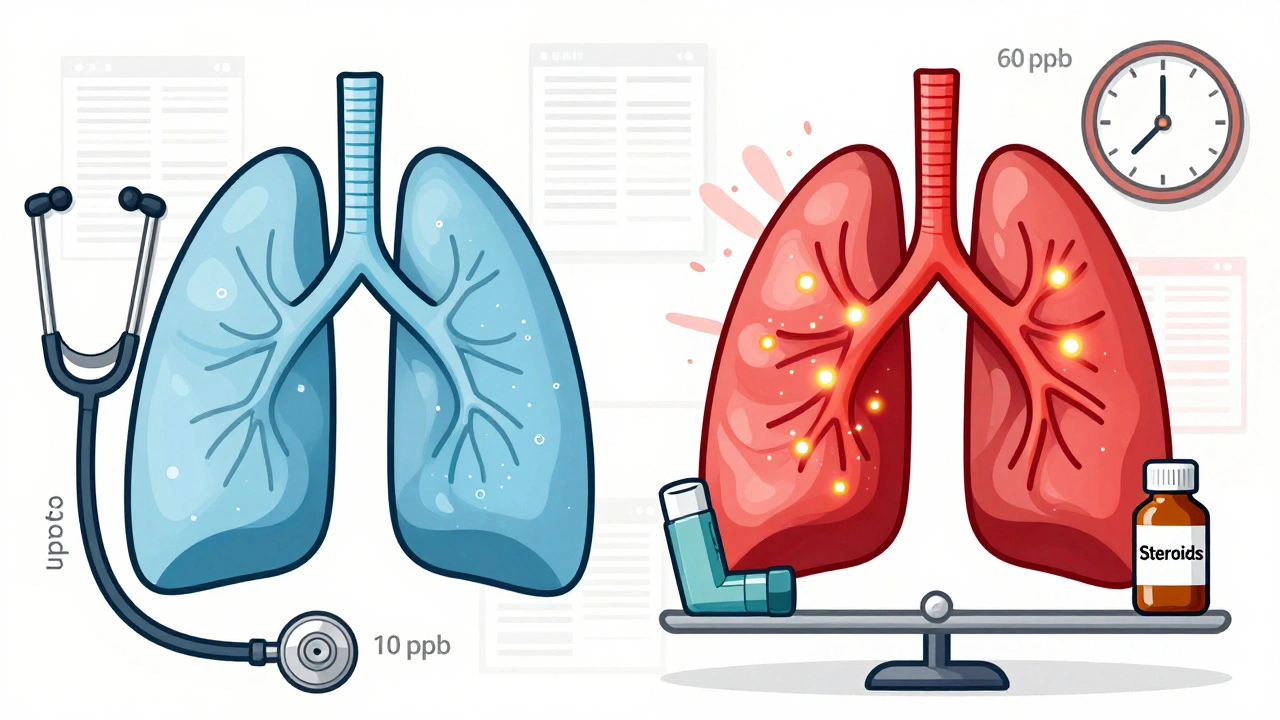
Doctors often rely on spirometry to diagnose asthma. But spirometry only shows if your airways are narrowed right now - not if they’re inflamed. Two people can have the same lung function test results, but one might have high inflammation (FeNO 60 ppb) and the other none (FeNO 10 ppb). That difference changes treatment.
Another option is a blood test for eosinophils. But that’s indirect. FeNO measures inflammation exactly where it matters - in your airways. Sputum tests (examining mucus) are even more accurate, but they’re messy, invasive, and hard to do in a clinic. FeNO gives you the same insight without the hassle.
Still, FeNO isn’t perfect. It won’t catch asthma caused by non-eosinophilic inflammation, like in some smokers or people with obesity-related asthma. That’s why it’s never used alone. It works best alongside symptoms, lung function tests, and medical history.
Who Benefits Most from FeNO Testing?
FeNO testing is especially helpful for:
- People with unclear asthma diagnosis - especially if symptoms don’t match lung test results
- Patients on controller inhalers who still have flare-ups
- Those being considered for biologic therapies (like dupilumab or benralizumab), which target specific inflammation pathways
- Children who can’t perform spirometry reliably
- People with allergic rhinitis who also have wheezing - to tell if it’s asthma or just nasal allergies affecting the lungs
One case from the American Lung Association involved a 34-year-old woman misdiagnosed with chronic bronchitis for seven years. Her FeNO level was 48 ppb - clear evidence of asthma. Once she switched to the right treatment, her symptoms vanished.
What Affects FeNO Results?
FeNO isn’t foolproof. Several things can throw off the reading:
- Smoking - cuts FeNO levels by 30-50%
- Recent use of inhaled steroids - can lower levels for days
- Eating, drinking (except water), or exercising within an hour before the test
- Allergic rhinitis or eosinophilic bronchitis - can raise FeNO even without asthma
That’s why timing matters. You should avoid food, drinks (other than water), smoking, and exercise for at least one hour before testing. And the test must be done before spirometry or using a rescue inhaler - otherwise, results won’t reflect true inflammation.
Real Patient Experiences
Patients who’ve had FeNO testing often say it was a turning point. On asthma forums, many share stories like:
- “Finally, objective proof my inhaler wasn’t working.”
- “My doctor realized I needed biologics - my FeNO was sky-high.”
- “It was easier than blowing into a spirometer. Took 30 seconds.”
But it’s not always smooth. Some face insurance denials. One user wrote: “My insurance denied it three times, even though I was in the ER twice last year.” In the U.S., coverage varies widely - Medicare covers it for asthma, but many private plans don’t. In the UK, where NICE guidelines require access, it’s routine. In rural U.S. clinics, only 22% offer it, compared to 67% in cities.

How Often Should You Get Tested?
For people on regular asthma medication, testing every 3-4 months helps track inflammation trends. If your doctor is adjusting your treatment - say, increasing your steroid dose or switching to a biologic - you might get tested more often. Once your asthma is stable, testing every 6-12 months is common.
Doctors use visual feedback tools on devices like the NIOX VERO® to make sure you’re exhaling correctly. This cuts down on invalid results from poor technique. With proper coaching, more than 95% of tests are usable.
The Future of FeNO Testing
FeNO technology is evolving fast. In early 2023, the FDA cleared the first smartphone-connected FeNO device - Breathometer Asthma - that lets patients test at home and share results with their doctor remotely. This could be a game-changer for people who live far from specialists or have trouble getting appointments.
Researchers are also studying how FeNO predicts response to expensive biologic drugs. If your FeNO is high, you’re more likely to benefit from these targeted therapies. That means fewer wasted treatments and lower costs.
But challenges remain. Standardization across devices is still inconsistent. And most studies have been done in white, Western populations. Ongoing trials like the NIH’s PREPARE-Asthma study are working to validate FeNO in diverse groups - including Black, Hispanic, and older adults - to make sure it works for everyone.
What to Do If Your Doctor Doesn’t Offer FeNO
If you think FeNO could help, ask. Say something like: “I’ve heard FeNO testing can show if my inflammation is under control. Can we check if it’s right for me?”
If your doctor says no, ask if they can refer you to an asthma specialist or allergist - these providers are more likely to use the test. You can also check with local academic hospitals or asthma clinics, which are far more likely to have the equipment.
And if insurance denies it, appeal. Provide documentation of frequent ER visits, hospitalizations, or uncontrolled symptoms. Many denials are overturned with the right paperwork.
FeNO testing isn’t magic. It won’t replace your inhaler or your doctor’s judgment. But it adds something powerful: objective data about what’s happening inside your airways. For many people, that’s the missing piece they’ve been waiting for.


Rashmin Patel
December 2, 2025 AT 07:16OMG this is SUCH a game-changer 🙌 I’ve had asthma since I was 8 and no one ever told me about FeNO until last year. My doctor finally ordered it after I kept having flare-ups despite ‘perfect’ spirometry results. My FeNO was 58 ppb - turns out my inhaler was basically useless because it wasn’t targeting the right inflammation. Now I’m on a biologic and I haven’t needed my rescue inhaler in 5 months. Why isn’t this standard everywhere?? 🤯
sagar bhute
December 3, 2025 AT 16:13This is just another overhyped medical fad pushed by Big Pharma. FeNO doesn’t even correlate reliably across devices. You’re better off just listening to your body and using your inhaler when you need it. All this tech just makes people paranoid and drains insurance.
Cindy Lopez
December 4, 2025 AT 08:52The article contains several grammatical inconsistencies. For instance, ‘you breathe in deeply through a filter that removes outside air’ - this phrasing is ambiguous. Does the filter remove outside air from the environment, or from the exhaled breath? Also, ‘FeNO levels are 25-50 ppb’ should be ‘FeNO levels range from 25 to 50 ppb.’ Minor, but matters in medical communication.
James Kerr
December 6, 2025 AT 03:30Just had my first FeNO test last week and it was so easy 😊 Like blowing out a birthday candle but slower. My number was 42 - my doc said it was a ‘classic asthma signal.’ I’d been on the same inhaler for 3 years thinking I was doing fine. Turns out I wasn’t. FeNO didn’t just give me data - it gave me peace of mind. If you’ve got asthma and still struggle, ask for it. No regrets.
shalini vaishnav
December 7, 2025 AT 14:54How can you trust a test developed in Western labs on predominantly white populations? In India, we have different asthma phenotypes - pollution-driven, not allergic. FeNO is irrelevant here. You can’t apply American guidelines to South Asian patients. This is colonial medicine disguised as innovation. We need local research, not imported gadgets.
Francine Phillips
December 8, 2025 AT 16:00My insurance denied it twice. I had to appeal with ER records. Took 3 months. They finally approved it. Worth it.
Katherine Gianelli
December 10, 2025 AT 03:35I’m a nurse in a rural clinic and we just got our first FeNO device last month - it’s like magic 🌟 We’ve got kids who’ve been labeled ‘wheezers’ for years, never got the right treatment. One 7-year-old had a FeNO of 67. Mom cried because she finally understood why her baby couldn’t run without gasping. This isn’t just tech - it’s hope in a handheld box.
Joykrishna Banerjee
December 12, 2025 AT 02:55While FeNO is indeed a biomarker of eosinophilic airway inflammation, its clinical utility is predicated upon a reductionist paradigm that fails to account for the pleiotropic nature of nitric oxide synthase isoforms, particularly iNOS upregulation in non-atopic phenotypes. Moreover, the NIOX VERO®’s calibration drift under variable humidity conditions introduces a systematic error margin of ±12%, rendering longitudinal comparisons statistically unreliable without rigorous standardization protocols - a caveat conspicuously absent from the article’s ‘future’ section.
Myson Jones
December 13, 2025 AT 05:48Thanks for sharing this. I’ve been thinking about asking my allergist about FeNO for months. After reading this, I’m going to bring it up next visit. No pressure, just… maybe it’s time to try something new.