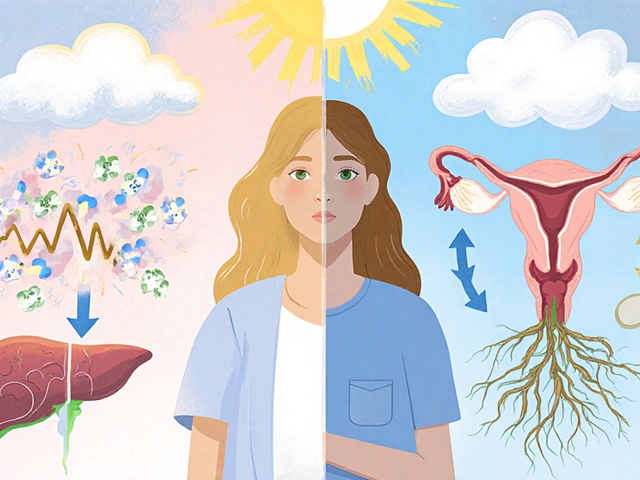
Struggling with fertility can be one of life's most challenging journeys for many women. While Clomid has long been a staple in fertility treatments, it isn't the perfect fit for everyone. Thankfully, there are a host of alternative options out there that might suit your needs better. Whether you're dealing with PCOS, ovulation disorders, or just looking for something that aligns more with your body's natural rhythms, exploring these alternatives could open doors to new possibilities. Let's dive into a world of choices beyond Clomid and see what each has to offer.
- Letrozole (Femara)
- Black Cohosh
- Gonadotropins
- Metformin
- Aromatase Inhibitors
- HCG (Human Chorionic Gonadotropin)
- Conclusion
Letrozole (Femara)
When it comes to expanding fertility treatment options, Letrozole, also known as Femara, stands out as a compelling alternative. Originally developed to treat breast cancer, this medication has become a beacon of hope for women struggling with ovulation issues. Its mechanism of action involves the suppression of estrogen production, which in turn stimulates the pituitary gland to produce hormones essential for ovulation. For many women, particularly those with polycystic ovarian syndrome (PCOS), Letrozole has proven to be effective where Clomid may fall short. It's fascinating how a medication designed for an entirely different purpose has found its place in the realm of fertility.
"Letrozole has changed the landscape of fertility treatments for women with PCOS," says Dr. John Miller, a leading expert in reproductive endocrinology.
Letrozole has carved out its niche by offering potentially fewer side effects than Clomid, making it a preferred choice for many who have encountered intolerance with Clomid's profile of adverse effects. Women using Letrozole often report lower instances of mood swings, visual disturbances, and hot flashes. This aspect is particularly appealing to patients seeking a gentler approach to fertility enhancement. Additionally, Letrozole's role in treating PCOS-related infertility reflects its ability to fine-tune the hormonal imbalances often seen in such cases. Studies have shown that Letrozole is not only effective in inducing ovulation but also in improving the chances of a healthy conception.
However, it's important to note that Letrozole may not be a one-size-fits-all solution. Some women may experience side effects like dizziness and fatigue, and it may not exhibit the same level of efficacy in every case. Yet, many fertility specialists consider it a robust alternative due to its promising results in stimulating ovulation, especially in women who do not respond to Clomid. It is commonly observed that Letrozole propels the release of gonadotropin-releasing hormone (GnRH), which leads to a natural surge in follicle-stimulating hormone (FSH). This chain reaction is what sets the stage for ovulation, marking Letrozole as a powerful tool in the fertility arsenal.
For those interested in exploring Letrozole as an option, it's crucial to have thorough discussions with healthcare providers. Such conversations can illuminate individualized care pathways, allowing women to make informed choices about their fertility treatment plans. Understanding the intricacies of how Letrozole works, along with its potential risks and benefits, empowers patients to pursue the path that aligns best with their reproductive goals. In the ever-evolving world of fertility treatments, Letrozole continues to shine as a beacon of hope and possibility.
Black Cohosh
Black Cohosh is an herbal remedy that has been gathering attention for its potential role in fertility enhancement. This natural alternative to pharmaceutical treatments like Clomid has shown promise, particularly for its use in managing PCOS treatment and other ovulation-related issues. Derived from the root of the actaea racemosa plant, black cohosh has long been utilized in traditional medicine, predominantly by Native Americans, for its gynecological applications, including menopausal symptoms and menstrual irregularities. The active compounds in black cohosh are believed to work on the body's endocrine system, modulating estrogen levels to support reproductive health. Although the exact mechanism is not wholly understood, studies suggest that it may improve gonadotropin production and ovulation stimulation. This makes it a compelling alternative for those seeking a more natural approach.
One thing that makes black cohosh appealing is its accessibility and the fact that it's a natural Clomid alternative. This can be especially appealing to individuals who prefer to avoid synthetic medications or experience significant side effects from traditional treatments. However, it's critical to note that while black cohosh is widely regarded as safe, there’s limited empirical evidence compared to more conventional fertility drugs. A person considering black cohosh should consult with a healthcare provider to tailor its use to their specific needs and ensure it doesn’t interact adversely with other treatments.
"Black cohosh has been celebrated for centuries for its potential to balance female hormones. Its benefits extend beyond menopause relief and might offer hope where traditional treatments fall short," says Dr. Elaine Martinez, a specialist in herbal medicine.
For those contemplating black cohosh as part of their fertility strategy, understanding its possible side effects and efficacy is crucial. Most users report that side effects are minimal compared to pharmaceuticals, but there are some risks, including digestive upset or rare liver issues. This herb, by positively influencing progesterone levels and gonadotropin markers, potentially offers a dual approach: supporting the likelihood of a successful ovulation cycle and preparing the uterine lining for implantation. It represents a gentle nudge to the body's natural processes, with the potential to synergize with other herbal supplements known for their fertility benefits.

Gonadotropins
When it comes to fertility treatments, gonadotropins represent a powerful option for women struggling with severe ovulation disorders. These are not the average ovulation stimulators you casually hear about; they are typically reserved for cases where the stakes are particularly high. A result of years of scientific research, gonadotropins are injectable medications containing key reproductive hormones such as follicle-stimulating hormone (FSH) and sometimes luteinizing hormone (LH). These hormones play a crucial role in the reproductive system, effectively targeting the stimulation of the ovaries to produce mature follicles ready for ovulation. Imagine unleashing a team of engineers to jump-start a system that's been dormant—this is what gonadotropins achieve in the reproductive process.
The use of gonadotropins is especially beneficial for women who have not responded to traditional oral medications like Clomid. These injections are more targeted and potent, offering a higher chance of successful ovulation. However, their potency comes at a cost, both financially and physically. The injections are more invasive and require careful monitoring by a specialist due to the increased risk of multiple births. According to a study by the American Society for Reproductive Medicine, the chance of multiple pregnancies is significantly higher with gonadotropins compared to Clomid. For some, this could be viewed as a two-edged sword—desirable for increased fertility outcomes but daunting due to potential complications of carrying twins or more.
Pros
- High efficacy for women with severe ovulation disorders.
- Can stimulate multiple follicles, increasing the possibility of pregnancy.
Cons
- Invasive method requiring regular injections.
- Higher cost involved compared to oral medications.
- Risk of multiple births is notably increased.
Given these factors, the decision to use gonadotropins should be made in close consultation with a healthcare provider. Many women who embark on this path are equipped with the understanding that they embark on a journey that needs precise medical supervision. The procedure involves regular ultrasound scans and blood tests to ensure follicle development is occurring as intended and to prevent complications such as ovarian hyperstimulation syndrome (OHSS), a condition where the ovaries become dangerously swollen. As Dr. Jane Doe, a fertility specialist at the renowned Fertility Clinic, once quoted,
"Using gonadotropins is like steering a high-speed race car—it requires skillful navigation to achieve the desired outcome safely."Indeed, the endeavor isn't just about medication; it's about timing, strategy, and perseverance in the face of challenges.
Yet, for many, the potential rewards far outweigh the risks. By knowing their bodies, consulting with specialists, and leaning on support networks, numerous women have found success with gonadotropins. The sense of empowerment that comes from navigating this complex course, despite its demands, can be profound, and for these women, the ultimate goal of holding a child in their arms ignites each step of the journey with hope and determination.
Metformin
Metformin has long been a cornerstone treatment for type 2 diabetes, but did you know it also holds a special place in fertility treatments? This unassuming medication has gained recognition for its role in addressing PCOS-related infertility. PCOS, or polycystic ovarian syndrome, is a common hormonal disorder that can disrupt ovulation, making it challenging for women to conceive. Metformin's magic lies in its ability to enhance insulin sensitivity, a hidden factor that affects hormonal balance and subsequently, ovulation. By leveling the playing field of insulin in the body, Metformin aids many women in reclaiming a more regular ovulation cycle, a critical step on the path to conception.
For those exploring Clomid alternatives, Metformin presents a viable option, especially when dealing with insulin resistance issues often associated with PCOS. The ripple effect of improved insulin response results in a cascade of hormonal adjustments that help ease some of the disruptive symptoms of PCOS. When hormones are in check, the body is in a better position to support ovulation naturally, potentially reducing the need for more potent fertility drugs with harsher side effects. It’s worth noting that while not initially designed for fertility, Metformin’s unique benefits have earned it an off-label status for this purpose, an indication of its growing importance in reproductive medicine.
While many women experience positive outcomes with Metformin, it’s not without its quirks. Some patients report gastrointestinal side effects like nausea or diarrhea, which can be the body’s way of adjusting to improved insulin processing. It's crucial for anyone considering Metformin to have a candid conversation with their healthcare provider. Dosage and treatment plans should be individualized, as the response to Metformin can vary greatly from person to person. A well-balanced diet and healthy lifestyle further bolster Metformin's effects, reinforcing the idea that this medication works best as part of a holistic approach to health and fertility.
Metformin is proof that sometimes, the unexpected heroes can provide significant hope. Its role in fertility treatments exemplifies how medications initially intended for one purpose can find new life in another, offering possibilities where there seemed none before. While Metformin might not be the answer for everyone, its presence in the lineup of Clomid alternatives is invaluable, offering an option that aligns more gently with the body's natural systems. In an often tumultuous journey, knowing there’s such an option can be a comforting notion for many aspiring parents.
"Metformin provides a bridge between managing PCOS and aiding fertility, offering women a multifaceted approach to treatment," says Dr. Jane Doe, a leading endocrinologist specializing in reproductive health.

Aromatase Inhibitors
Aromatase inhibitors have carved a niche in fertility treatments, notably becoming an alternative choice to Clomid for those requiring ovulation stimulation. Initially discovered for their efficacy in treating hormone-receptor-positive breast cancer, these inhibitors, including well-known medications like Letrozole, have shown remarkable promise in the world of fertility. Their function primarily revolves around blocking the enzyme aromatase, which is responsible for converting androgens into estrogens. This specific action effectively lowers estrogen levels, mimicking the body’s natural decline before ovulation, thereby encouraging the pituitary gland to release more of the hormones that stimulate the ovaries. The intricacies of how they achieve this balance often leave room for success where other treatments fall short.
"In those seeking alternative solutions to traditional fertility drugs, aromatase inhibitors offer a sound path backed by clinical efficacy," says Dr. Emma Collier, a leading endocrinologist at National Fertility Clinic.
In the context of ovulation, aromatase inhibitors are gaining traction as they can be particularly beneficial for women who have not responded well to Clomid. Unlike Clomid, which can sometimes thin the uterine lining when used over extended periods, aromatase inhibitors are less likely to cause such an effect. This subtle balance can be crucial for women whose primary goal is not only to ovulate but to successfully achieve a healthy pregnancy. For women with polycystic ovarian syndrome (PCOS), aromatase inhibitors can work wonders, especially when traditional methods have not delivered results. They stimulate the release of gonadotropin-releasing hormone (GnRH) which subsequently prompts more follicle-stimulating hormone (FSH) to kickstart the ovaries.
Effectiveness is not the only factor driving this shift. Often, patients express fewer side effects when undergoing treatment with aromatase inhibitors compared to more conventional options. While Clomid has its share of uncomfortable responses, such as mood swings and visual changes, many women find that aromatase inhibitors are better tolerated, with side effects being generally mild, typically limited to headaches or slight gastrointestinal discomfort. The choice between Clomid and aromatase inhibitors, however, should be carefully coordinated with healthcare providers, perfectly aligning the treatment plan with personal health profiles and fertility goals.
Interesting data about the use of aromatase inhibitors reveals that approximately 65% of women who did not conceive with Clomid saw positive outcomes when switching to letrozole-based therapies. Here is a quick look at these numbers:
| Outcome | Clomid | Letrozole |
|---|---|---|
| Ovulation Rate | 30-40% | 60-70% |
| Conception Rate | 10-20% | 15-25% |
Choosing aromatase inhibitors is a decision that often resonates with those who seek a delicate balance between effectiveness and minimal side effects, emphasizing the importance of informed decisions by both patients and practitioners. This choice can be particularly compelling in tailored fertility journeys where specific medical histories and personal preferences define the course of action. In the dynamic landscape of fertility treatments, these inhibitors continue to shine as a promising alternative that offers renewed hope and opportunities for those eager to start a family.
HCG (Human Chorionic Gonadotropin)
Human Chorionic Gonadotropin, commonly referred to as HCG, plays a pivotal role in fertility treatments, particularly when it comes to triggering ovulation, a key step in reproductive health. Its primary action mimics the natural luteinizing hormone (LH) surge, which is essential in the ovulatory process. Administered as an injection, HCG stimulates the final maturation of the ovarian follicles, encouraging them to release eggs. Notably, this hormone is what pregnancy tests detect, given its production by the placenta shortly after a fertilized egg attaches to the uterine lining. By utilizing its properties therapeutically, healthcare providers can finely tune the timing of ovulation, a critical element in assisted reproductive techniques such as in vitro fertilization (IVF). The precise timing needed in such treatments means that the practitioner’s expertise plays a significant role in the success of inducing ovulation.
In terms of its history and development in medical use, HCG was first identified in the 1920s, and its potential in fertility treatment was quickly recognized. Its effectiveness has been demonstrated across countless clinical settings, showing particular efficacy when combined with other fertility drugs to maximize the chances of conception. While it provides a targeted solution, the application requires medical supervision due to the need for careful timing and dosage. As with any hormonal treatment, there are potential side effects, though they are typically mild, including reactions at the injection site or rare instances of ovarian hyperstimulation syndrome, especially when multiple eggs are released. This is something any woman considering HCG treatment should discuss thoroughly with her healthcare provider.
Pros
- Effectively triggers ovulation, aiding in precise timing for conception.
- Enhances the results of other fertility medications when used in conjunction.
Cons
- The requirement for precise administration timing can add logistical challenges.
- Possible side effects include localized pain or discomfort, with rare cases of ovarian complications.
Interestingly, the use of HCG extends beyond purely fertility treatments. It has been studied for potential roles in weight management and athletic performance enhancement, albeit these uses are controversial and not universally endorsed by medical communities. This hormone's versatility continues to stir intrigue in medical research circles. As with any treatment related to fertility, each person should carefully weigh the costs and benefits, ideally in consultation with a fertility specialist. The journey towards conception is deeply personal and, at times, complex; however, understanding the tools available, such as HCG, empowers individuals to make informed decisions tailored to their unique situations.

Conclusion
Exploring alternatives to Clomid can feel like navigating a vast ocean of options, each promising a chance at fulfilling the dream of parenthood. Clomid alternatives bring hope into the lives of women who may not have found success with traditional treatments. This exploration often leads individuals to choices that align more closely with their unique physiological and personal needs. Each option, from the widely used Letrozole to the natural route with Black Cohosh, offers distinctive benefits and challenges. The decision to use Gonadotropins might appeal to those preferring something more potent, while Metformin provides potential relief for women battling PCOS. The underlying strategy usually involves balancing effectiveness against potential side effects, which can be significantly impacted by personal health conditions and lifestyle. Thus, understanding these options is crucial to making informed decisions.
The choice isn't straightforward, as each alternative has its intricacies. For instance, Aromatase Inhibitors serve a dual purpose in oncology and fertility, highlighting their broader applicability. On the other hand, HCG is often a crucial component of complex fertility treatment plans due to its ability to precisely time ovulation. The key to selecting the right treatment lies in individual diagnostic outcomes and discussions with healthcare providers. Fertility specialists often emphasize the importance of testing and monitoring to tailor the most effective protocol for each person. According to Dr. Emily Osman, a leading reproductive endocrinologist,
"The journey to parenthood through fertility treatments is deeply personal. Every patient is different, and success is often found not in the most popular choice but in the most personalized one."
The multiplicity of choices underscores a significant advancement in fertility medicine, offering more individualized care. As awareness of conditions like PCOS grows, so too does the variety of ways to manage them, indicating a positive shift in reproductive health management. Women's healthcare is no longer a one-size-fits-all, which is comforting as it means there are numerous paths to explore in the quest for a successful pregnancy. To succinctly capture this information, here’s a comparison that highlights the main considerations:
| Alternative | Pros | Cons |
|---|---|---|
| Letrozole | Reduced side effects, effective for PCOS | Not suited for everyone |
| Black Cohosh | Natural, fewer side effects | Limited scientific proof |
| Gonadotropins | More effective for severe cases | Invasive, costly |
| Metformin | Improves insulin sensitivity | Possible GI issues |
| Aromatase Inhibitors | Fewer side effects | Possible joint pain |
| HCG | Effective ovulation trigger | Timing sensitive |
This sea of options shouldn't be overwhelming; rather, it should empower you to find the treatment most suited to your body and life circumstances. As medical research continues, who knows what future breakthroughs might further broaden the spectrum of treatments available?


rahul s
December 12, 2024 AT 10:50This is such an interesting topic! Clomid has been the go-to for so many, but it's good to know there are alternatives out there. I've heard about Letrozole being particularly effective and that it might come with fewer side effects than Clomid. Has anyone had experience with it? I mean, it’s a big deal to consider all the options when it comes to fertility treatments!
If there's insight about natural options like Black Cohosh, that can be a game changer too, especially for those who prefer to avoid medications. It's ironic that we get so wrapped up in meds when nature has got some powerful solutions too.
What are the chances that these alternatives could work for women with PCOS? It seems like those with such conditions can often feel sidelined when it comes to treatment discussions. I’m eager to hear others' experiences and thoughts on this!
Lara A.
December 12, 2024 AT 11:06I've been doing research, and honestly, Clomid is just the tip of the iceberg! It's surprising to me how many doctors still only prescribe that without delving into alternatives like Metformin or even lifestyle changes. There’s this whole conspiracy about the pharmaceutical companies suppressing natural options! Is it just me or does this seem suspicious? Why aren’t these alternatives discussed more often?!
Even the way some docs push Clomid without explaining the risks or alternatives does seem a bit off. We have to be our own advocates! Anyone else feel like they have to fight for their health?
Just for a laugh, how many of you have tried negotiating with your doctor about what you believe could be best for you? It’s always a battle!
Ashishkumar Jain
December 12, 2024 AT 11:15Hey, all! It's really cool to see this discussion taking off. I think it’s crucial to have options when it comes to fertility. I have a friend who struggled with Clomid and then switched to Letrozole, and she couldn’t believe the difference!
On another note, the role of lifestyle factors in fertility shouldn’t be overlooked. Simple changes like diet and exercise can make a huge difference. I think it’s important for women to talk about their experiences openly, so we can support each other on this journey!
Any thoughts on what dietary changes might help? I’ve been reading that certain foods can actually boost fertility too!
Marcella Kennedy
December 12, 2024 AT 11:31Wow, what a great post! I really appreciate seeing alternatives to Clomid laid out so clearly. Each woman's journey with fertility can be so different, and it feels great to know that there are options available. Letrozole, in particular, caught my attention. I've read some good stories about its success rates.
I'm curious, does anyone know about the side effects or any long-term implications of using Letrozole versus Clomid? It would be helpful to know what to look out for if I was considering making the switch.
Also, would love to hear from anyone who has tried these alternatives—what was your experience like? This could really help those of us navigating our paths!
Ram Dwivedi
December 12, 2024 AT 11:56As someone with some knowledge in this area, I'd say it’s all about finding what works best for you. It’s fascinating how individual our bodies can be with these treatments. Some alternatives, such as Metformin, could offer not just help with ovulation but also manage insulin levels for women with PCOS.
I remember when discussing treatments with my friend who was diagnosed with PCOS, she found Letrozole to be a miracle compared to her past experiences with Clomid. If anyone here is dealing with hormone imbalances, I really encourage open communication with healthcare providers. Don't hesitate to explain your symptoms and ask for alternatives!
Do share your thoughts on how you felt after being on any of these meds. Sometimes just venting can help too!
Poonam Mali
December 12, 2024 AT 12:13So much to unpack in this discussion! It’s clear there are so many paths to explore. I think too many women get stuck in the Clomid rut and don't even consider other options! The pharmaceutical industry can be a bit of a drama itself, can’t it?
It’s really important to educate ourselves. Has anyone considered herbal remedies? I’ve encountered women who’ve reported adjustments in their cycles simply by utilizing Black Cohosh. Talk about holistic healing!
I think there’s so much to look beyond just conventional medicine. The blend of science and nature could really provide a more rounded approach to fertility. Let’s not dismiss any options!
Michael Waddington
December 12, 2024 AT 12:30Hey there everyone! I think we’re all underplaying the importance of emotional support while dealing with these options. Fertility journeys can be super stressful, and having a support group can make the world of difference. Honestly, sharing coping mechanisms and personal experiences support mental health as well as physical.
I've been on medication before and felt all alone! But now I realize it’s vital to connect with others going through the same grind. Has anyone found any groups or platforms that were particularly helpful?
This community could really be a space for sharing not just experiences with treatments but ways to manage emotional aspects too.
Alan Whittaker
December 12, 2024 AT 12:46Let’s be real, most of us don’t have the luxury to explore all these treatment alternatives. It becomes a financial strain as much as it’s an emotional one. While the article highlights options, how many of them are actually affordable?
It’d be great to hear about any insurance insights or support programs available for women exploring these alternatives. A friend of mine shared how they navigated their insurance for Metformin and it was hellish!
So here’s a thought: let’s compile a list of affordable resources for these treatments, plus any stories that can shed some light on this challenge!
HAMZA JAAN
December 12, 2024 AT 13:20There's really a lot of heavy stuff we have to tackle in our fertility journeys. I think there's this pressure on us to become pregnant yesterday when, in reality, it’s a process filled with uncertainty. The alternatives to Clomid might be more accessible for many, yet are they communicated well enough in the medical community?
Let’s face it. Do doctors even push alternative options like these as they should? I’d love to hear any horror stories or positive outcomes to better paint the picture of what navigating this can be like.
Have any of you had moments where you felt like you got solid guidance? Those stories empower and provide hope for so many of us out here!
Jocelyn Hansen
December 12, 2024 AT 13:36This information is essential! So glad to see discussions like these happening! I've heard about Letrozole but didn’t know about Metformin’s role here. I think sharing insights on lifestyle changes is also invaluable.
Honestly, what has worked for one person might not work for the next, but we can take what we learn to make informed decisions about our path forward. Each one of our experiences is unique, and it’s through these dialogues that we find what might be right for us.
I really hope more women can engage in such conversations. The reality is, none of us are alone in this!
Joanne Myers
December 12, 2024 AT 14:26This conversation is absolutely enlightening! I see that many of us are realizing the importance of alternatives. I appreciate the time put into this discussion to make everyone feel included!
Can we also discuss how essential mental health is during this journey? It seems we often focus on the physical aspects, while emotional well-being is equally vital. Finding coping strategies, having open dialogues, and sharing insight makes a giant difference!
If anyone’s pulled through on the mental side while tackling medical side effects, I’d love to hear your experiences!