Ovulation PCOS: Understanding Fertility, Symptoms, and Management
When you have polycystic ovary syndrome, a common hormonal disorder that disrupts ovulation and causes irregular periods. Also known as PCOS, it doesn’t just mean cysts on the ovaries—it means your body struggles to release an egg each month, making it harder to get pregnant. If you’re trying to conceive and your cycle is unpredictable, you’re not alone. About 1 in 10 women of childbearing age have PCOS, and most of them don’t ovulate regularly—or sometimes at all.
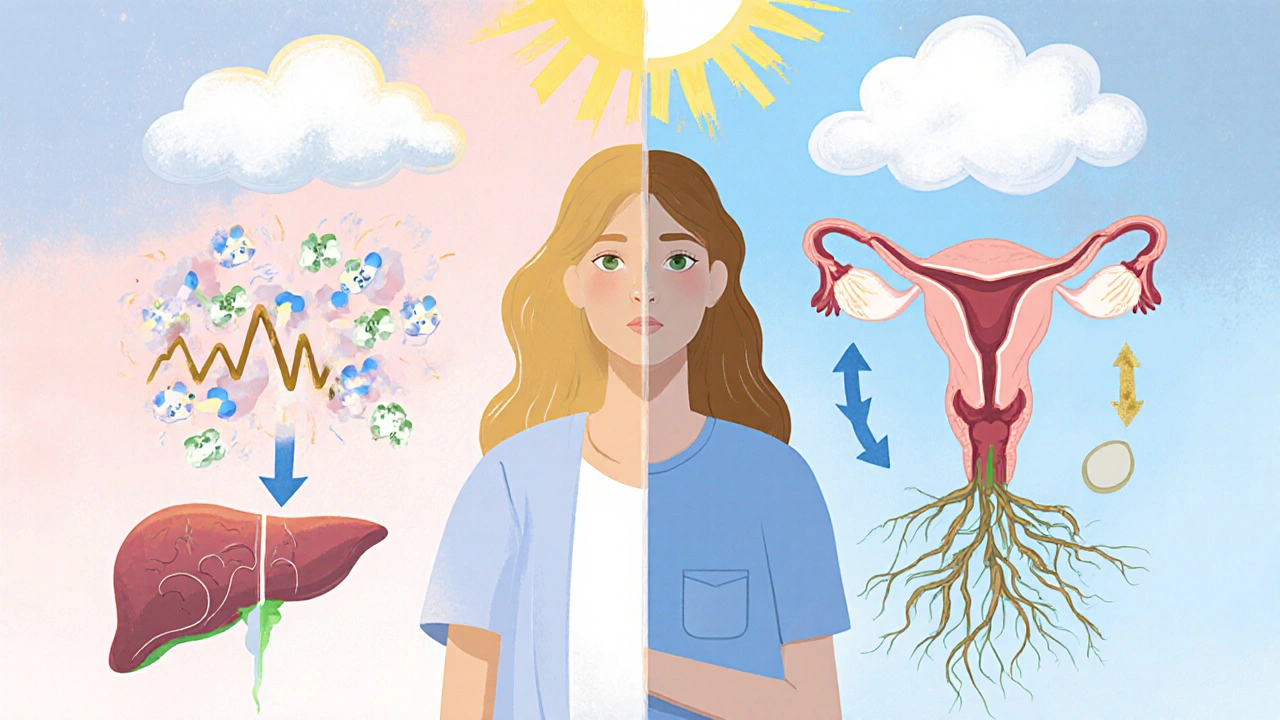
The real problem behind missed ovulation isn’t just hormones—it’s often insulin resistance, when your cells don’t respond well to insulin, causing blood sugar to spike and triggering excess male hormones. That spike in testosterone and other androgens shuts down the ovary’s ability to mature and release an egg. It’s not about being overweight, though that can make it worse. Even thin women with PCOS can have insulin resistance and no ovulation. And because your body thinks it’s under stress, it holds back ovulation like a survival move.
That’s why so many women with PCOS get stuck in a loop: no period, no ovulation, no pregnancy, and more frustration. But here’s the thing—it’s not hopeless. Tracking basal body temperature, using ovulation predictor kits, and even simple lifestyle changes like eating fewer refined carbs can help restart ovulation. Some women respond to metformin, a diabetes drug that improves insulin sensitivity. Others need clomiphene or letrozole to trigger ovulation. And yes, weight loss helps—but only if it’s sustainable. You don’t need to lose 50 pounds. Losing 5% of your body weight can bring back regular cycles for many.
What you won’t find in most guides is how often PCOS gets misdiagnosed. Some women are told they have PCOS because they have acne or hair growth, but their cycles are normal. Others have real ovulation issues but no cysts on ultrasound—yet still have PCOS. The diagnosis isn’t about one test. It’s about the pattern: irregular periods, high androgens, and no other cause like thyroid disease or high prolactin.
The posts below give you real, practical tools to navigate this. You’ll find guides on tracking ovulation with simple methods, how certain meds affect fertility in PCOS, why some supplements help and others don’t, and how to avoid common mistakes when trying to conceive. You’ll see what works for real women—not just theory. Whether you’re just starting out or have been trying for months, these posts cut through the noise and give you what you need to take control.
Metformin for PCOS: How It Boosts Ovulation and Insulin Sensitivity
Metformin helps women with PCOS ovulate by improving insulin sensitivity, lowering testosterone, and restoring menstrual cycles. It's cheaper and safer than many fertility drugs, with added benefits for long-term metabolic health.
November 21 2025