Kaposi Sarcoma Risk Assessment Tool
Select your risk factors below to assess your potential risk for Kaposi Sarcoma:
Kaposi Sarcoma lesions typically appear as:
Select your risk factors and click "Assess My Risk" to see your risk level.
Treatment Overview
Effective treatment combines:
- Antiretroviral therapy (ART) for HIV
- Local therapies for lesions
- Systemic chemotherapy if needed
Most people infected with HHV-8 never develop KS. The virus requires a weakened immune system to trigger tumor formation.
Early detection and sustained immune health dramatically improve prognosis.
| Modality | Best For | Typical Outcome | Key Side Effects |
|---|---|---|---|
| Antiretroviral Therapy (ART) | HIV-associated KS | Lesion regression in 70-80% within 6-12 months | GI upset, metabolic changes |
| Local radiation | Isolated skin or oral lesions | Rapid shrinkage, pain relief | Skin irritation, fatigue |
| Cryotherapy or laser ablation | Small, superficial nodules | Complete clearance in 60-70% cases | Scarring, pigment changes |
| Systemic chemotherapy | Extensive cutaneous or visceral disease | Overall response ~50%, disease control 12-18 months | Myelosuppression, cardiotoxicity |
When you hear the term Kaposi Sarcoma, you might picture rare skin spots or a disease linked only to celebrities. In reality, it’s a vascular tumor that can affect anyone with a weakened immune system, most commonly people living with HIV. This guide breaks down what Kaposi Sarcoma is, why it appears, how doctors spot it, and what you can do about it.
Key Takeaways
- Kaposi Sarcoma (KS) is caused by infection with human herpesvirus8 (HHV‑8) and thrives when immunity is low.
- Typical KS lesions start as painless purple or brown patches on skin, but they can also involve internal organs.
- Diagnosis relies on visual exam, biopsy, and tests for HHV‑8 DNA.
- Effective treatment combines antiretroviral therapy (ART) for HIV, local therapies for lesions, and sometimes systemic chemotherapy.
- Early detection and sustained immune health dramatically improve prognosis.
What Exactly Is Kaposi Sarcoma?
Kaposi Sarcoma is a cancer of the blood‑vessel lining that manifests as vascular tumors on the skin, mucous membranes, and sometimes internal organs. First described by Moritz Kaposi in 1872, KS was once considered a rare disease of elderly Mediterranean men. The AIDS epidemic in the 1980s revealed a second, far more aggressive form linked to immune suppression.
How Does HHV‑8 Trigger the Tumor?
Human herpesvirus8 (HHV‑8), also called Kaposi’s sarcoma‑associated herpesvirus, is the essential driver of KS. The virus integrates into endothelial cells, prompting them to proliferate and produce new blood vessels - a process known as angiogenesis. HHV‑8 is a gamma‑herpesvirus transmitted mainly through saliva, sexual contact, and blood products. Most infected people never develop KS; only when the immune system can’t keep the virus in check does the tumor emerge.
Who Is at Risk?
The biggest risk factor is a compromised immune system. Here’s a quick snapshot:
- People living with HIV/AIDS: Up to 30% of untreated individuals develop KS.
- Organ transplant recipients: Immunosuppressive drugs raise risk; KS accounts for ~1% of post‑transplant cancers.
- Elderly men of Mediterranean or Eastern European descent: Classic KS appears slowly, often limited to the lower limbs.
- Children in sub‑Saharan Africa: Endemic KS occurs without HIV, linked to high HHV‑8 prevalence.
Spotting the Signs: Common Symptoms
KS lesions are often the first clue. They can be:
- Flat, pink, purple, or brown patches that may be raised or nodular.
- Located on the legs, feet, face, or oral cavity.
- Accompanied by swelling (edema) if lymphatic vessels are blocked.
When internal organs are involved, symptoms vary:
- Gastrointestinal KS: abdominal pain, nausea, or occult bleeding.
- Lung involvement: shortness of breath, cough, or chest pain.
- Rarely, lymph node enlargement or neurological signs if the brain is affected.
Because lesions are painless, they’re often missed until they grow or cause functional problems.
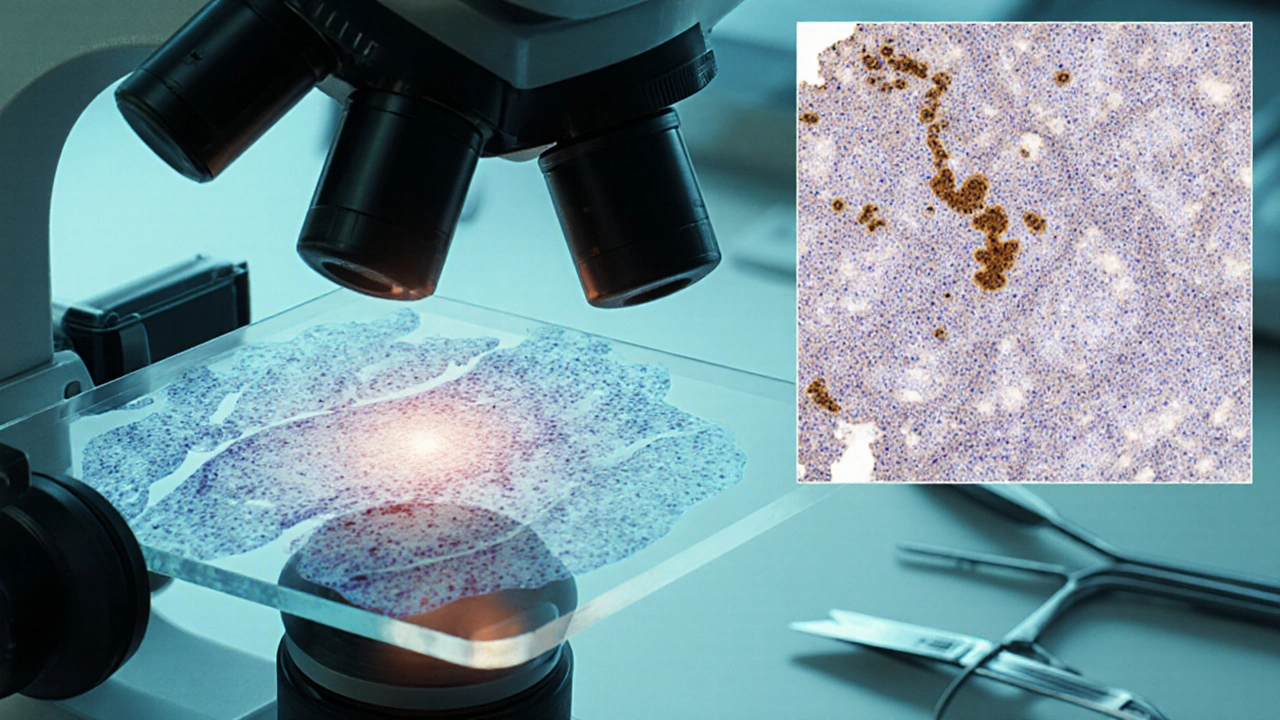
How Doctors Diagnose Kaposi Sarcoma
The diagnostic pathway blends visual assessment with laboratory confirmation:
- Clinical examination: Dermatologists look for the characteristic purplish lesions.
- Skin or tissue biopsy: A tiny sample is stained and examined under a microscope for spindle‑shaped cells and vascular channels.
- Immunohistochemistry: Tests for HHV‑8 latent nuclear antigen (LANA‑1) confirm viral involvement.
- Imaging studies: Endoscopy, CT, or MRI scans assess internal organ spread if symptoms suggest.
- Laboratory tests: CD4 count and HIV viral load gauge immune status; HHV‑8 PCR may be utilized in research settings.
The combination of histology and HHV‑8 detection provides a definitive diagnosis.

Treatment Options: From Local to Systemic
Therapy is tailored to disease extent, immune health, and patient preferences. Below is a concise comparison of the main approaches.
| Modality | Best For | Typical Outcome | Key Side Effects |
|---|---|---|---|
| Antiretroviral Therapy (ART) | HIV‑associated KS | Lesion regression in 70‑80% within 6‑12 months | GI upset, metabolic changes |
| Local radiation | Isolated skin or oral lesions | Rapid shrinkage, pain relief | Skin irritation, fatigue |
| Cryotherapy or laser ablation | Small, superficial nodules | Complete clearance in 60‑70% cases | Scarring, pigment changes |
| Systemic chemotherapy (e.g., liposomal doxorubicin) | Extensive cutaneous or visceral disease | Overall response ~50%, disease control 12‑18 months | Myelosuppression, cardiotoxicity |
| Immunomodulators (e.g., interferon‑α) | Patients with stable immune function | Variable response, often combined with ART | Flu‑like symptoms, depression |
In HIV‑positive patients, getting onto effective ART is the cornerstone; viral suppression often leads to KS regression without extra chemotherapy. For transplant recipients, reducing immunosuppression can trigger remission but must be balanced against graft rejection risk.
Living With Kaposi Sarcoma: Practical Tips
Managing KS isn’t just about medicine. Here are everyday strategies that help maintain skin health and overall well‑being:
- Skin care: Keep lesions clean, avoid friction, and use gentle moisturizers to prevent cracking.
- Regular follow‑ups: Schedule dermatology visits every 3‑6 months, especially after starting or changing therapy.
- Nutrition: A balanced diet supports immune recovery; foods rich in antioxidants (berries, leafy greens) may aid skin healing.
- Exercise: Moderate activity improves circulation and can reduce edema associated with KS lesions.
- Psychological support: Joining HIV or KS support groups reduces isolation and provides coping tools.
While the disease can be emotionally taxing, many people achieve long‑term remission with the right medical and lifestyle plan.
Prognosis: What the Numbers Say
Overall survival depends heavily on immune status and disease spread. In the ART era, the 5‑year survival for HIV‑related KS approaches 80% when patients maintain CD4 counts above 200 cells/µL. Classic KS in older adults tends to be indolent, with life expectancy similar to age‑matched peers. Conversely, rapid‑progressing epidemic KS in untreated AIDS patients historically carried a median survival of less than 1 year.
Key prognostic factors include:
- CD4 count and HIV viral load (higher CD4, lower load = better outlook).
- Extent of visceral involvement (lung or GI disease worsens prognosis).
- Response to first‑line therapy (early regression predicts longer remission).
Frequently Asked Questions
Can Kaposi Sarcoma be cured?
There is no single cure, but many patients achieve complete remission, especially when immune function is restored with ART. Ongoing monitoring is essential because lesions can recur if immunity wanes.
Is HHV‑8 infection alone enough to cause KS?
No. Most people infected with HHV‑8 never develop KS. The virus needs a permissive environment-typically a weakened immune system-to trigger tumor formation.
Do skin patches of KS bleed or itch?
Lesions are usually painless and non‑pruritic, but they can ulcerate or bleed if traumatized. Any sudden change warrants a medical review.
Can I get KS from casual contact?
Casual, non‑skin‑to‑skin contact (e.g., handshake) does not spread HHV‑8. Transmission mainly occurs via saliva, sexual activity, or blood products.
How often should I see my doctor after a KS diagnosis?
Initial follow‑up is usually every 1-2 months to assess treatment response. Once stable, visits taper to every 3-6 months, with imaging if internal disease was present.
Understanding Kaposi Sarcoma empowers you to recognize warning signs, seek timely care, and partner with clinicians on an effective treatment plan. Whether you’re newly diagnosed or supporting a loved one, staying informed makes a tangible difference in outcomes.


Zach Westfall
October 8, 2025 AT 14:24Kaposi sarcoma is a vascular tumor that thrives in weakened immune systems.
It is caused by the human herpesvirus 8 that hangs around endothelial cells.
The virus alone is not enough it needs the body to be compromised.
Patients living with HIV are the most well‑known group to develop KS.
Organ transplant recipients on immunosuppressants are also at risk.
Typical lesions appear as purple or brown patches on the skin.
They can also hide in the mouth or internal organs causing hidden trouble.
Diagnosis usually starts with a skin exam followed by a biopsy that reveals spindle cells.
Immunohistochemistry for HHV‑8 LANA‑1 confirms the viral presence.
Staging the disease involves imaging studies to see if internal organs are involved.
First‑line therapy for HIV‑associated KS is antiretroviral treatment which restores immune function.
Lesions often regress once the viral load is suppressed and CD4 counts rise.
Local therapies such as radiation, laser, or cryotherapy are options for isolated lesions.
Systemic chemotherapy becomes necessary when disease is widespread or visceral.
Overall prognosis hinges on immune recovery, disease extent, and how quickly treatment starts.
Pranesh Kuppusamy
October 17, 2025 AT 03:44One cannot ignore the hidden networks that facilitate the spread of HHV‑8 beyond the scope of conventional epidemiology.
The interplay between pharmaceutical interests and the under‑reporting of Kaposi sarcoma cases suggests a deliberate obfuscation.
When immune systems are deliberately weakened, either by medication or policy, the virus finds fertile ground.
Thus the rise of KS in certain regions may not be a mere coincidence but a symptom of larger systemic manipulation.
It is imperative to scrutinize the data presented by health agencies for potential bias.
Only through vigilant analysis can we hope to expose the true dimensions of this disease.
Crystal McLellan
October 25, 2025 AT 17:04i read that HHV‑8 is spread thru saliva and some ppl think it’s only a problem for AIDS but that’s just the tip of the iceberg
the real issue is how immunosuppressive drugs are handed out without proper oversight
people on those meds end up gettin KS and no one seems to care
its like the medical industry is playing hide and seek with the truth
Kelly Thomas
November 3, 2025 AT 05:24Hey there! If you’re navigating a Kaposi sarcoma diagnosis, remember you’re not alone – many have walked this path and emerged stronger.
First off, get your HIV viral load under control with ART; the immune rebound can shrink lesions dramatically.
Pair that with regular dermatology check‑ups to catch any new spots early.
For skin lesions, options like laser ablation or cryotherapy provide quick cosmetic relief.
Don’t forget nutrition – omega‑3 rich foods and antioxidants support healing.
Stay active, stay positive, and keep a solid support network; you’ll be amazed at how resilience fuels recovery.
Mary Ellen Grace
November 11, 2025 AT 18:44Just wanted to say that KS can be really scary but catching it early makes a huge diffrence.
Make sure you keep your appointments and follow the doc’s advice.
Also try to keep skin moisturized so it doesnt get irritated.
Carl Watts
November 20, 2025 AT 08:04Reading your comprehensive rundown on Kaposi sarcoma reminds me of the delicate balance between chaos and order within the human body.
When the immune system falters, the virus exploits that void, much like a philosophical paradox where the absence of protection births pathology.
It’s a stark illustration of how interconnected our physiological systems truly are, and why holistic care matters.
Brandon Leach
November 28, 2025 AT 21:24Wow thanks for the pep talk.
Alison Poteracke
December 7, 2025 AT 10:44It’s good to focus on both treatment and everyday care – staying on ART and monitoring skin changes are key steps.
Marianne Wilson
December 16, 2025 AT 00:04The previous comment incorrectly claims “omega‑3 rich foods and antioxidants support healing” without citing any peer‑reviewed evidence; such statements should be qualified with “may” or omitted entirely to avoid misinformation.
Patricia Bokern
December 24, 2025 AT 13:24OMG the way KS can just pop up out of nowhere is freaky af – it’s like the virus is waiting in the shadows ready to strike when you least expect it, and the whole system seems rigged to let it happen!
Garrett Gonzales
January 2, 2026 AT 02:44From a clinical oncology perspective, the integration of HAART with adjunctive locoregional modalities constitutes a multimodal therapeutic algorithm that optimizes both virologic suppression and oncologic control, thereby enhancing progression‑free survival metrics.
Aman Deep
January 10, 2026 AT 16:04The veil between disease and destiny blurs when we contemplate HHV‑8 as a catalyst for transformation – a silent whisper urging cells to reshape themselves into vascular tapestries :) the mind ponders the unseen forces that guide such metamorphosis.
Herman Bambang Suherman
January 19, 2026 AT 05:24Maintain your ART regimen, schedule regular dermatology visits, and monitor any new lesions promptly.
Meredith Blazevich
January 27, 2026 AT 18:44I can feel the weight of uncertainty that comes with a KS diagnosis – the fear, the hopes, the endless “what‑ifs” swirling like storm clouds.
Knowing that early intervention can dramatically alter outcomes offers a sliver of light amid the gloom.
Lean on your support network, cherish each small victory, and remember that medical science continues to advance, bringing new therapies to the forefront.
Your resilience is a powerful ally in this battle.
Nicola Gilmour
February 5, 2026 AT 08:04Take one step at a time – each appointment, each medication dose, each moment of rest builds momentum toward recovery.
Darci Gonzalez
February 13, 2026 AT 21:24Stay hopeful and keep fighting, every day brings new possibilities for improvement :)
Kelly Larivee
February 22, 2026 AT 10:44Keeping a consistent treatment schedule and staying in touch with your healthcare team makes a big difference.