Left Ventricular Failure – What It Is and How to Manage It
If your heart’s main pumping chamber starts to struggle, you might hear doctors talk about left ventricular failure (LVF). Simply put, it means the left side of the heart can’t push blood out strong enough to meet the body’s needs. That sounds scary, but understanding the basics helps you stay on top of it.
Common Signs & Symptoms
People with LVF often notice a few tell‑tale clues:
- Shortness of breath: Even light activity or lying flat can make breathing feel hard.
- Fatigue: You get tired quickly because muscles aren’t getting enough oxygen.
- Swelling (edema): Ankles, feet, or even the abdomen may puff up as fluid builds up.
- Rapid or irregular heartbeat: The heart tries to compensate for weak pumping.
- Persistent cough: Often dry, sometimes with pink‑tinged sputum.
If you spot these signs, especially together, it’s worth talking to a doctor right away. Early detection can keep the condition from getting worse.
Treatment & Lifestyle Tips
Doctors treat LVF with a mix of medicines, lifestyle tweaks, and sometimes procedures. Here’s what you’re likely to hear about:
- Medications: ACE inhibitors or ARBs relax blood vessels; beta‑blockers slow the heart down; diuretics help shed excess fluid.
- Monitoring: Regular weight checks catch fluid buildup early. A sudden jump of two pounds in a day should raise an alarm.
- Diet changes: Cut back on salt, which traps water, and keep portion sizes moderate to avoid extra strain.
- Exercise: Light activities like walking or stationary cycling improve heart efficiency. Start slow and let your doctor set safe limits.
- Quit smoking & limit alcohol: Both stress the heart and can worsen LVF.
In some cases, doctors might suggest devices such as a pacemaker or an implantable defibrillator to keep rhythms steady. If medicines don’t help enough, surgery like valve repair or even a heart transplant could be options – but those are rare and only after other routes fail.
Living with LVF also means staying on top of routine check‑ups. Blood tests, echo scans, and sometimes stress tests let your care team see how the heart’s performing and adjust treatment quickly.
Remember, LVF is a chronic condition, not a one‑time event. Keeping track of symptoms, sticking to medication schedules, and making small daily choices can make a big difference in quality of life. If you ever feel dizzy, chest pain, or sudden swelling, treat it as an emergency – call your doctor or head to the nearest ER.
Bottom line: left ventricular failure means the heart’s left pump isn’t working at full strength. Knowing the signs, following medical advice, and adopting heart‑friendly habits puts you in control of the condition rather than letting it control you.
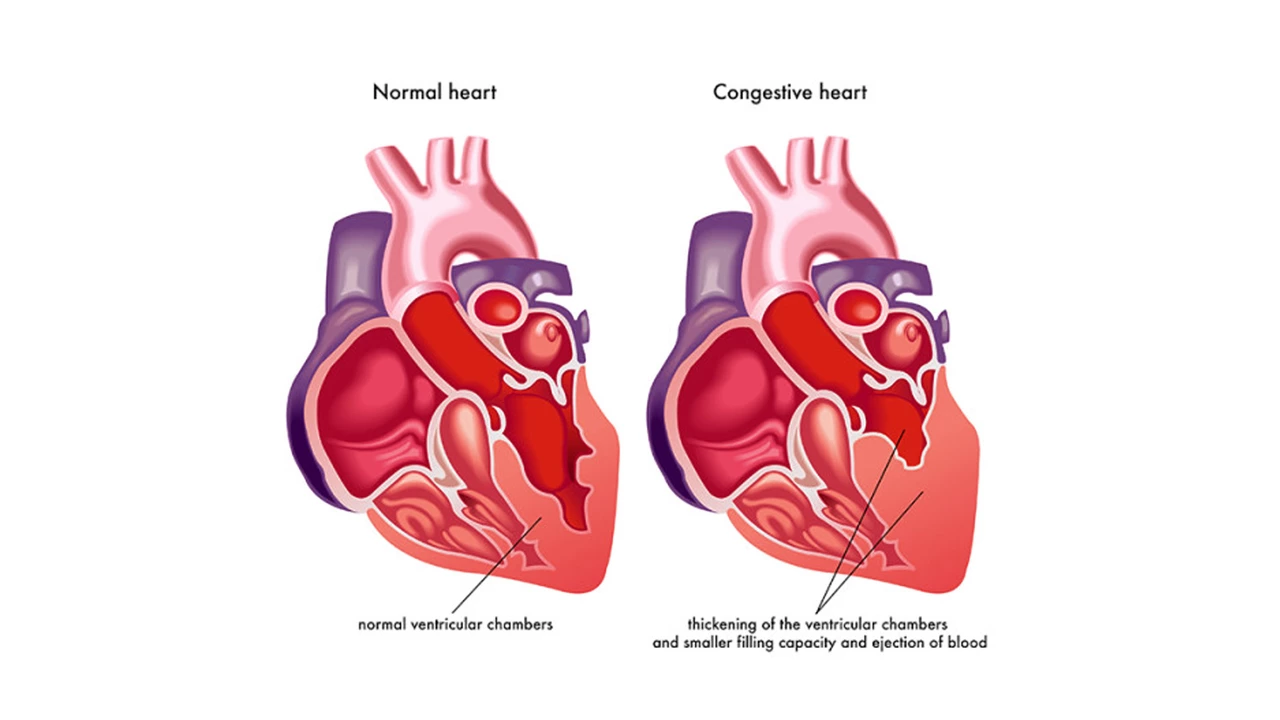
The Science Behind Left Ventricular Failure: How the Heart Muscle Weakens
In my latest blog post, I delved into the science behind left ventricular failure, a condition where the heart muscle weakens and struggles to pump blood efficiently. Researchers have found that various factors like heart attacks, high blood pressure, and infections can damage the heart muscle, leading to this condition. As the heart weakens, it can enlarge and become less effective at pumping blood, causing symptoms like shortness of breath and fatigue. Treatment options vary depending on the severity, but can include medications, lifestyle changes, and in some cases, surgery. It's crucial to understand and recognize the signs of left ventricular failure to ensure timely treatment and prevent further complications.
May 8 2023